Neuroradiology
Neuroradiology focuses on imaging and therapies to diagnose and to treat disorders of the adult and pediatric brain, spine, neck, and central and peripheral nervous system. The UCSF neuroradiology group is comprised of internationally recognized experts in every one of these disciplines, and in the latest state-of-the-art imaging with CT, MRI, MEG and molecular modalities such as PET. The group has expertise in the full array of neurologic disease, including brain tumors, stroke and other vascular disorders, spine disease, neurodegenerative diseases, and brain malformations. With 12 full-time neuroradiologists across our campuses, we are one of the largest divisions of neuroradiology in the United States.
Adult and Pediatric Neuroimaging
Neuroradiololgy Expertise
Patients are referred to UCSF neuroradiology from all over the world. Each year we perform and interpret over 14,000 CTs, 22,000 MRIs, 250 myelograms, more than 1,000 diagnostic angiograms, over 650 interventional procedures, and more than 500 spinal procedures including biopsies, nerve root block, epidural injections of steroids and specialized procedures including vertebroplasty and kyphoplasty. For example, we offer special expertise and apply advanced cutting edge MRI techniques for the diagnosis and monitoring of patients with brain, skull base and ENT tumors, traumatic brain injuries, the range of pediatric brain and spine disorders as well as for patients with spine related pain. Because we perform an unusually high number of procedures each year, referred from a variety of specialists, we have gained enormous clinical and scientific expertise. That expertise leads to more precise diagnoses and better clinical judgment and skill. It also directly facilitates our ability to help patients and their doctors by sharing our skills in “seeing,” detecting, and treating abnormalities. This allows us to provide informative consultations to referring physicians and to suggest proper interventions.
Collaborative Approach
At UCSF neuroradiology we foster close collaboration with the physicians who refer to us: experts in Adult and Pediatric Neurology, Neurological Surgery, Pediatrics, Oncology, Otolaryngology, Primary Care/Internal Medicine, Orthopedic Surgery, and Radiation Oncology. We regularly work with physicians in the greater community as well as with physicians at UCSF. We also discuss difficult patient issues at a variety of multidisciplinary conferences with treating physicians, which allows us to recommend the best care plan to our patients.
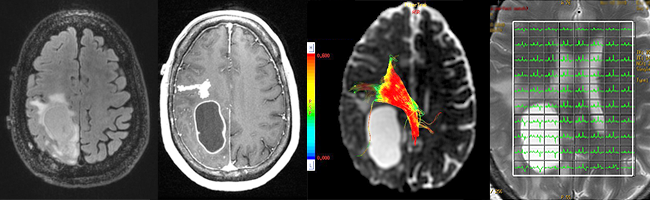
Neuroradiology Advanced Techniques and Technologies
At UCSF we have the highest quality imaging equipment and use the appropriate one for the task at hand in order to achieve crisper, better, more detailed, higher resolution images for patients.





























