Clinical & Translational Musculoskeletal Imaging
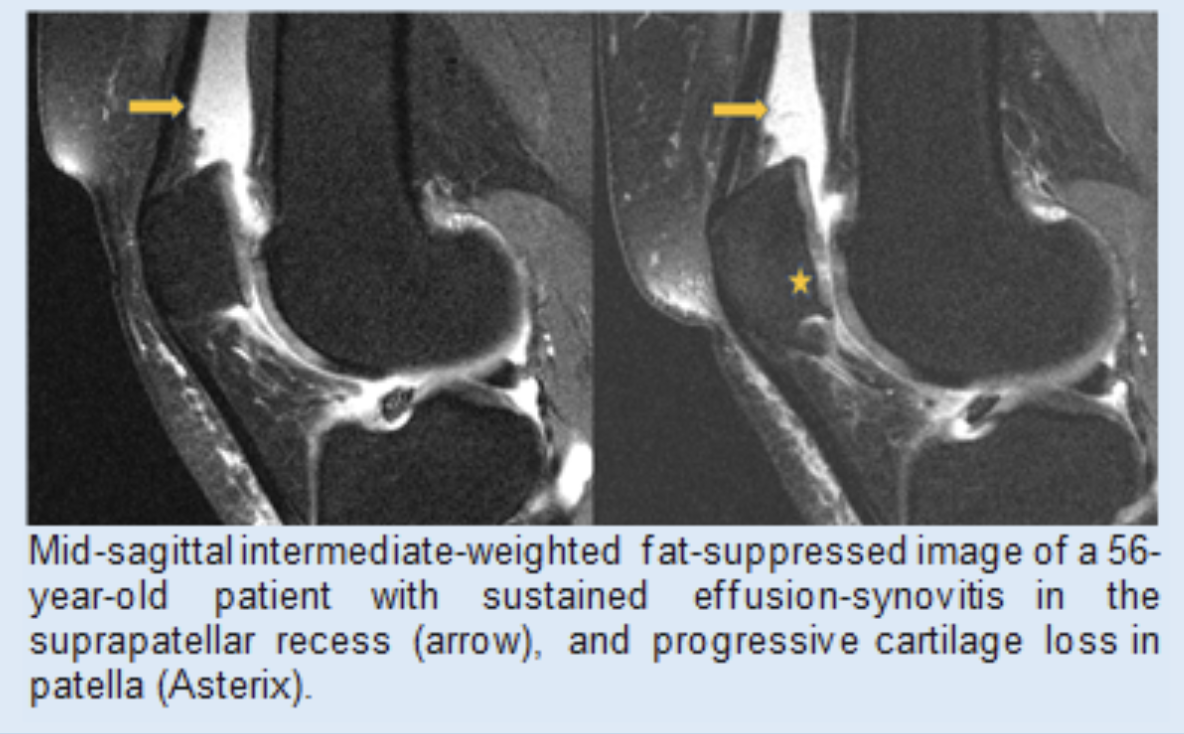
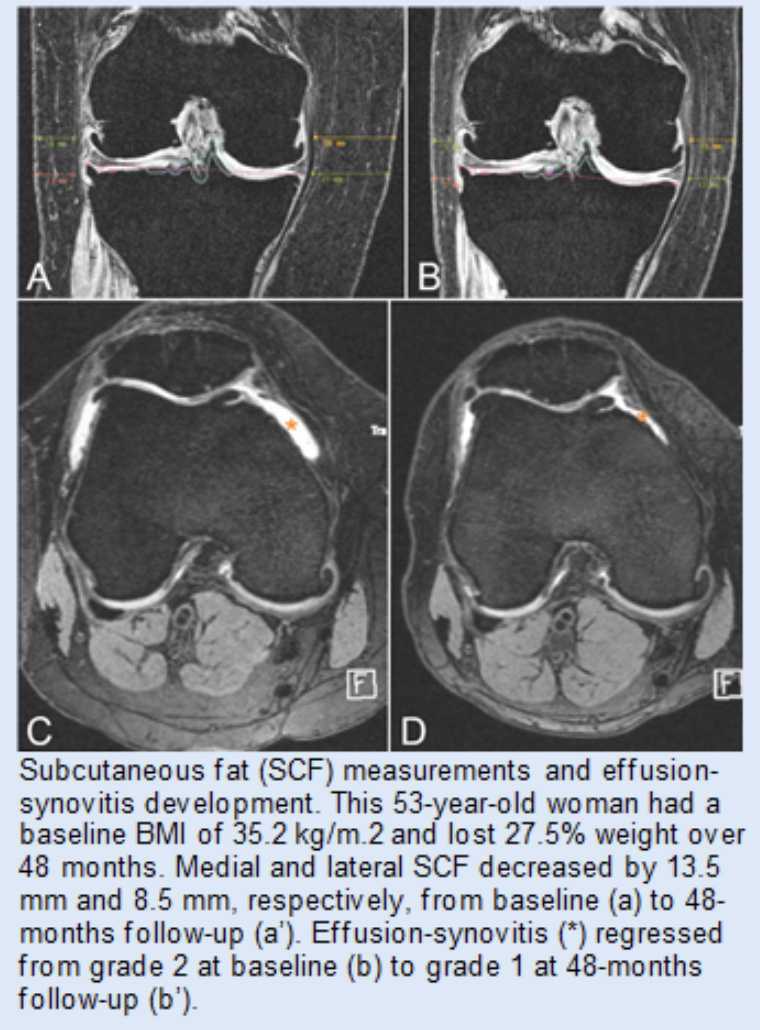
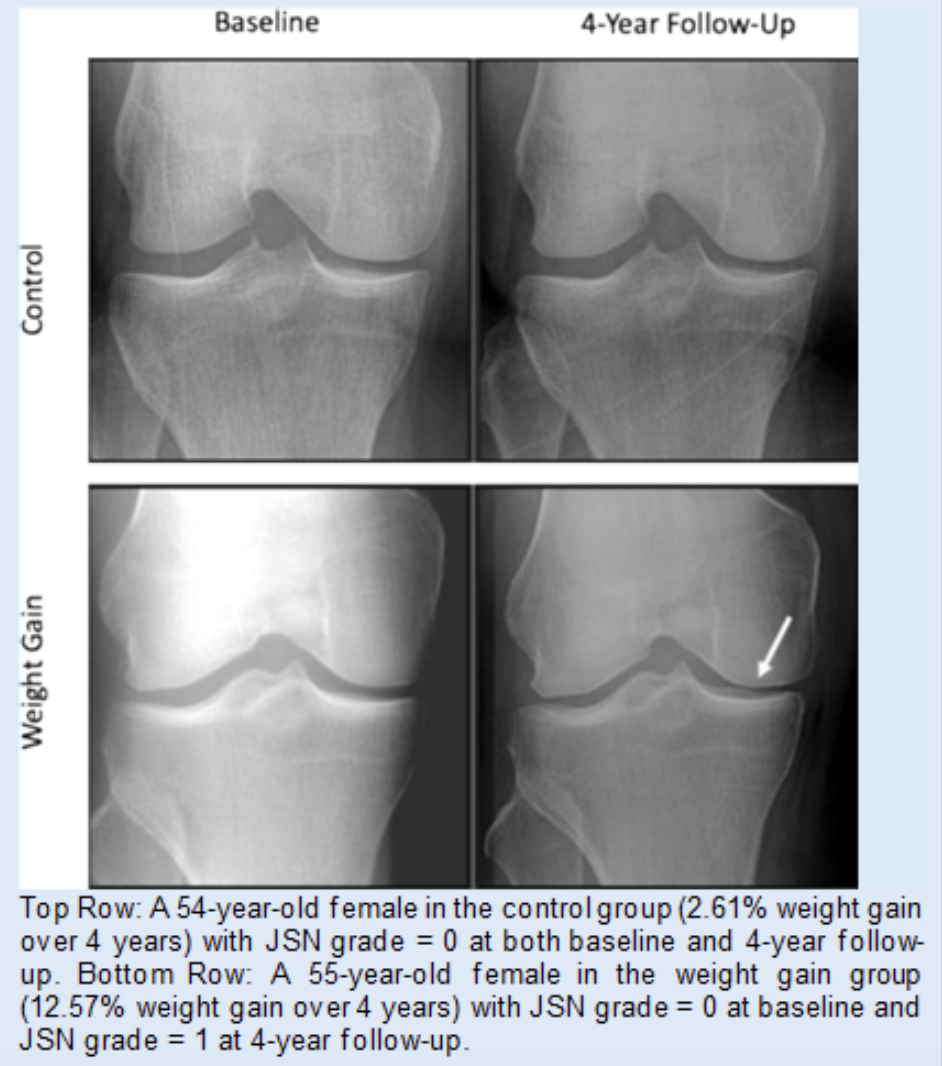
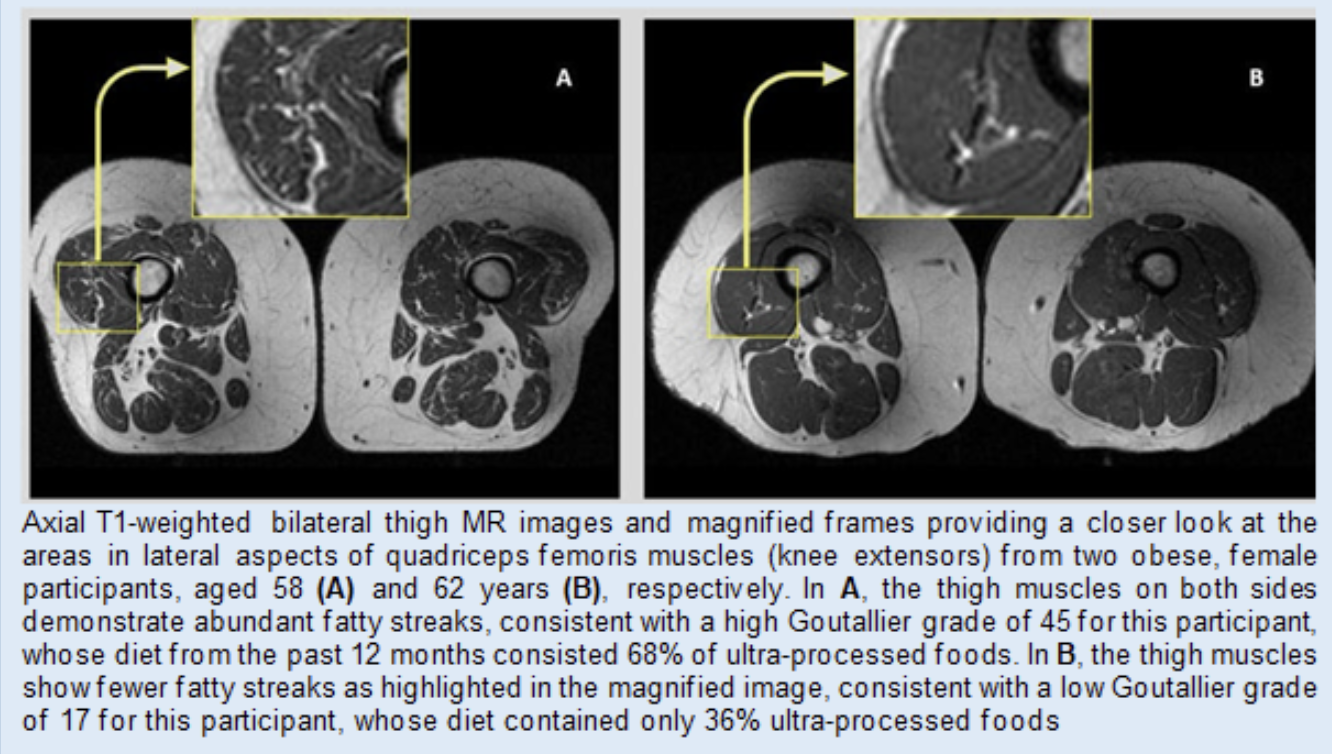
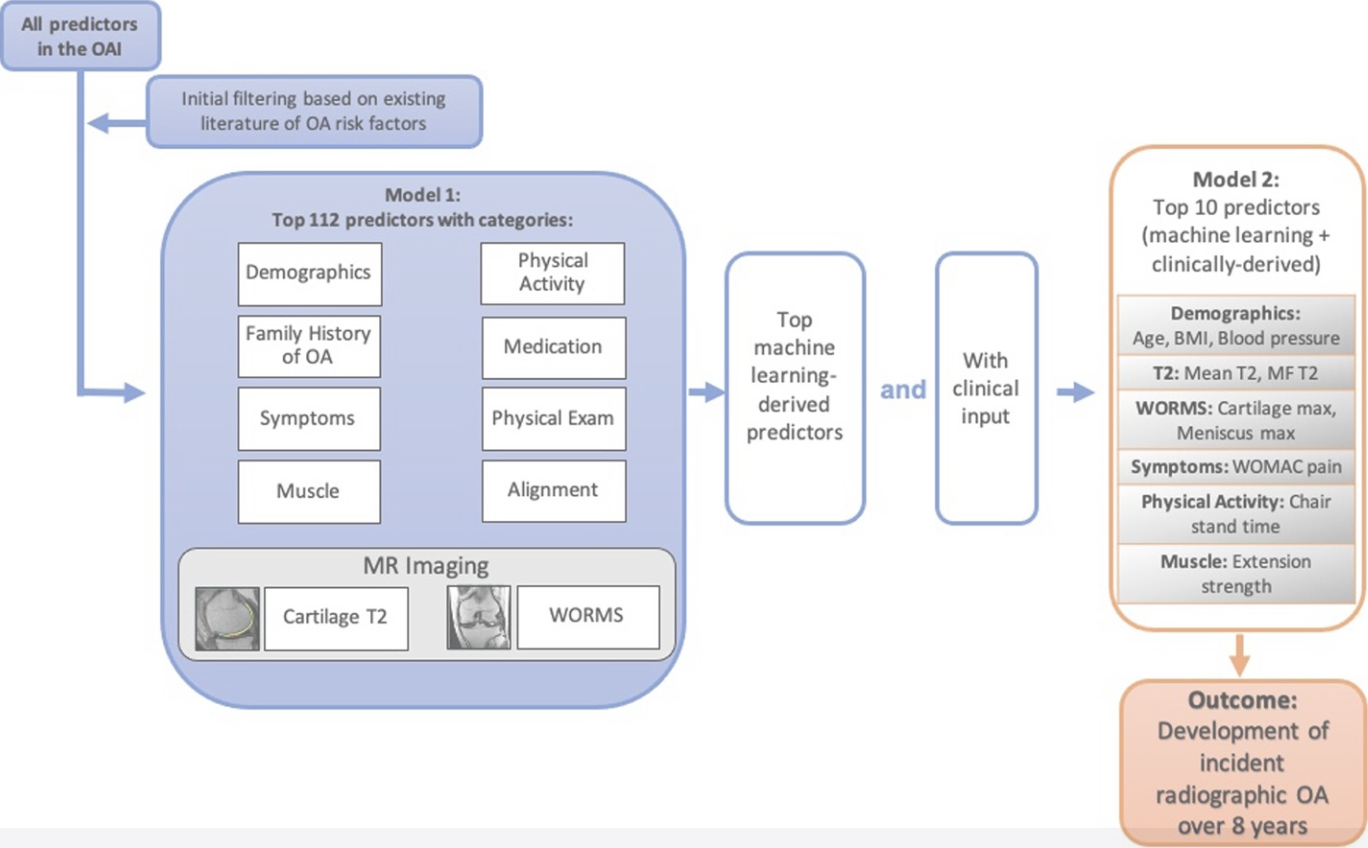
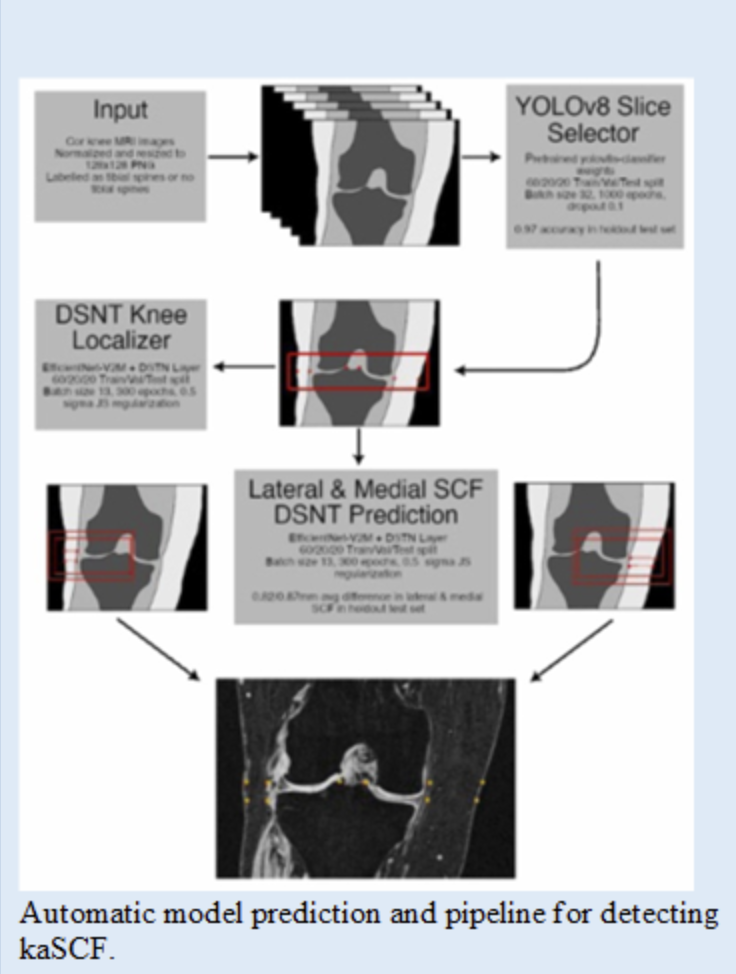
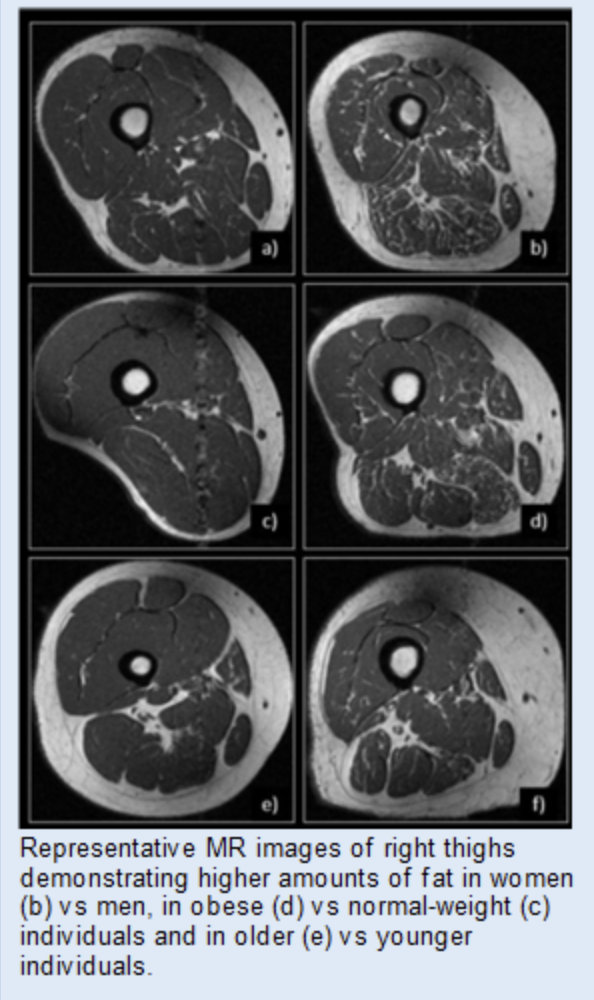
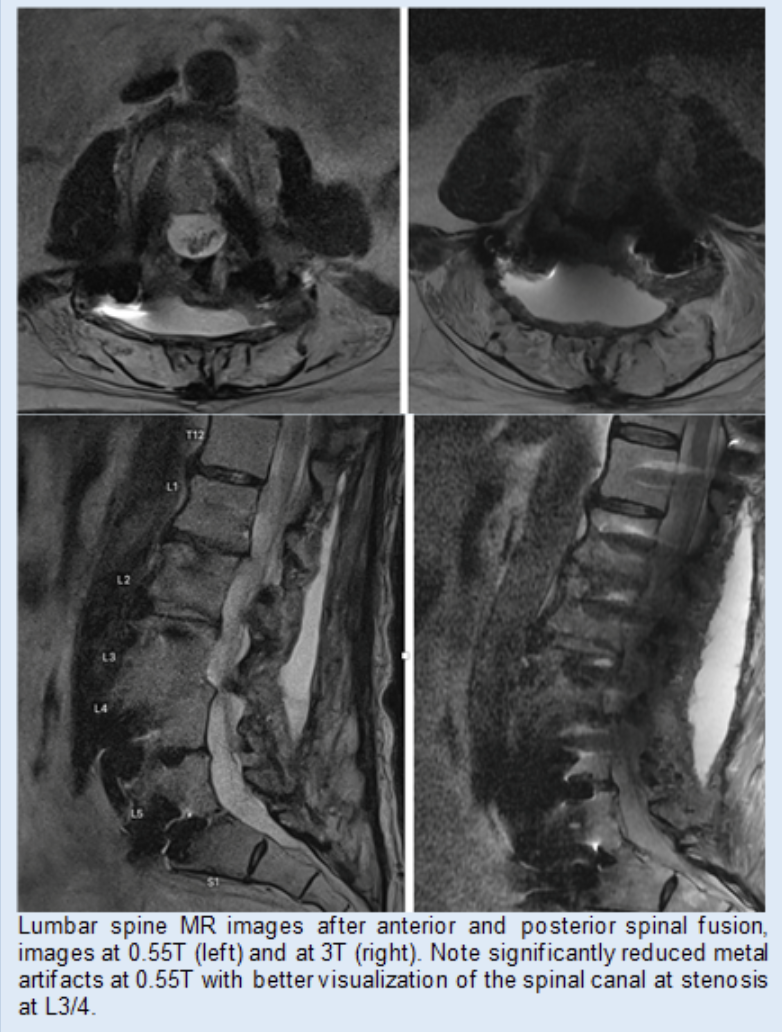
The Clinical and Translational MSK Imaging group (CTMI) uses standard and novel imaging techniques to study abnormalities of the musculoskeletal system. Our focus is on imaging biomarkers in osteoarthritis; the team has developed quantitative and semi-quantitative measurement tools to assess and monitor disease severity. These include Whole-Organ Magnetic Resonance Imaging Scores (WORMS) of the knee, composite scores to measure knee joint synovitis, and the Scoring Hip Osteoarthritis with MRI (SHOMRI) system to study the hip. In addition, artificial intelligence-based tools to measure muscle volume and fat infiltration, periarticular adipose tissue, and synovitis volume have been developed. Recently, we also investigated novel MR imaging techniques to reduce metal artifacts, low field MRI at 0.55T, and CT-like MR imaging techniques.
Led by Dr. Thomas M. Link, Musculoskeletal Imaging Division Chief, and Dr. Gabby Joseph, the biostatistician of the team, the group consists of clinician scientists, bioengineers, epidemiologists, and computer scientists. Our overarching goal is to improve patient care by developing imaging biomarkers that can predict disease progression sensitively or serve as outcomes for early disease stages. Research is funded by the National Institutes of Health, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, and industry sponsors.
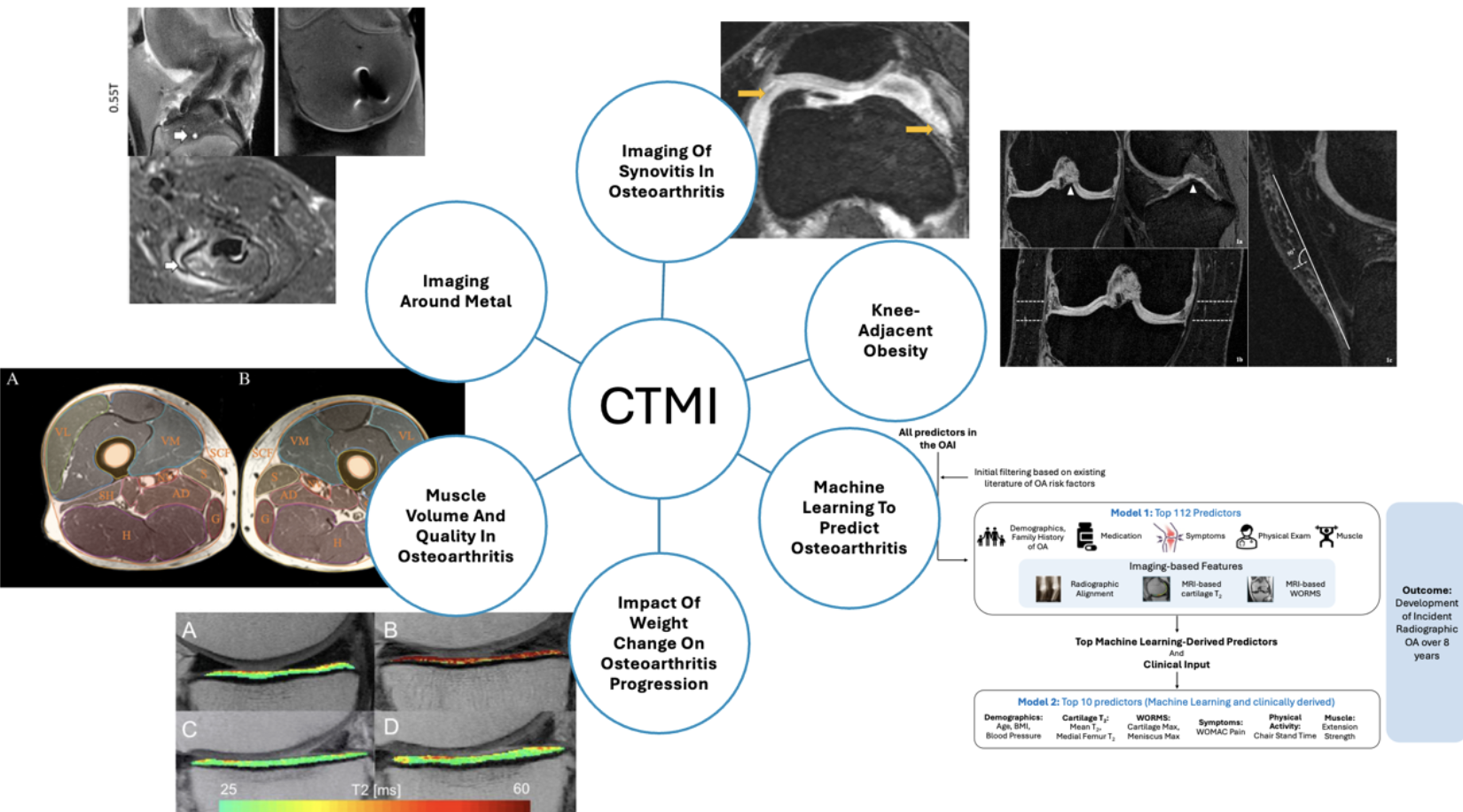
Research Projects
Publications
See a complete list of the group’s publications at Dr. Link’s UCSF profile.