Focused Ultrasound in Bone/ Musculoskeletal (HIFU)
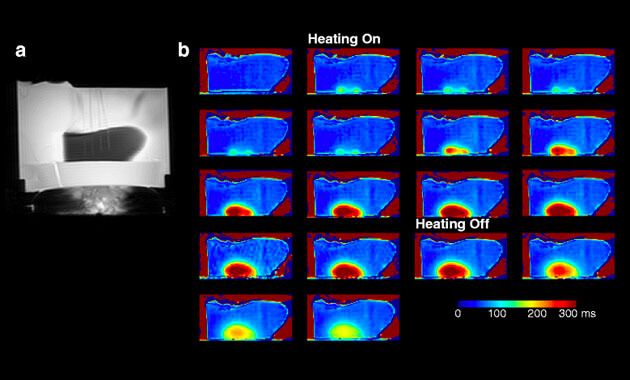
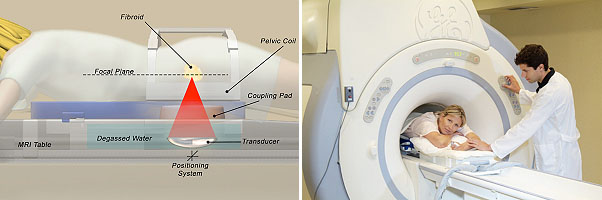
HIFU stands for "High-Intensity Focused Ultrasound." It is also known as MRgFUS (MRI-guided focused ultrasound) and FUS (focused ultrasound). HIFU is an innovative, non-invasive treatment for a wide range of tumors and diseases. HIFU uses an ultrasound transducer, similar to the ones used for diagnostic imaging, but with much higher energy. The transducer focuses sound waves to generate heat at a single point within the body and destroy the target tissue. The tissue can get as hot as 150-200°F in just 20 seconds. This process is repeated as many times as is necessary until the target tissue is destroyed. MRI images are used to plan the treatment and monitor the degree of heating in real time.
What are the benefits of Bone/Musculoskeletal HIFU?
- Non-invasive non-surgical treatment
- Lower treatment risks
- No ionizing radiation
- Faster recovery time
- Precision
Clinical Indications
We are currently treating patients with the following indications:
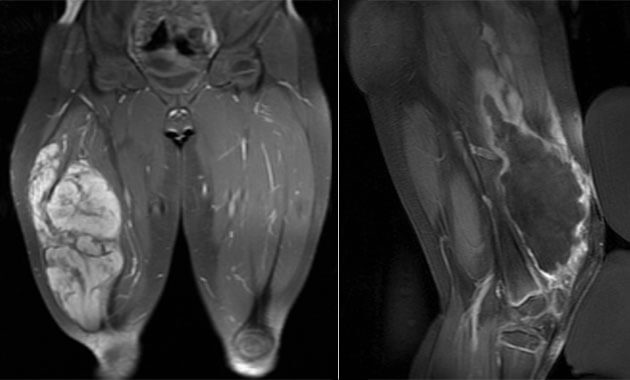
- Desmoid tumors
- Osteoid osteomas
- Bone metastases
- Undifferentiated pleomorphic sarcomas
- Essential Tremor
- Prostate cancer
HIFU Clinical Research Trials
HIFU is FDA-approved for treatment of metastatic bone pain. UCSF offers clinical treatments for bone metastases and desmoid tumors which are billed to patient insurance.
We also have two ongoing clinical research trials for patients with osteoid osteomas and undifferentiated pleomorphic sarcomas. For more information regarding these two research trials, please contact our Clinical Research Coordinator, Maya Aslam at [email protected].