Osteoid Osteoma Treated with Minimally Invasive Technique of Radiofrequency Ablation
Osteoid osteoma is a benign tumor of the bone. This tumor is most frequently found in the legs but may occur also at other bones in nearly any part of the body. Osteoid osteoma is a tumor of children and young adults, it is very rare in older adults over the age of 50.
Diagnosing an Osteoid Osteoma
Osteoid osteoma causes a lot of pain in almost all patients. This pain is most frequently in the night, and patients sometimes wake up from the pain. The pain may also occur during the day. Sometimes the pain gets worse over time. It may only be dull, but sometimes also very sharp and gets worse with activity.
Typically patients have relief of their pain with aspirin, ibuprofen or other anti-inflammatory agents.
There may be a lot of inflammation around the tumor and the soft tissue around the tumor may be painful or swollen. Sometimes even a lump may be felt.
Imaging of Osteoid Osteoma
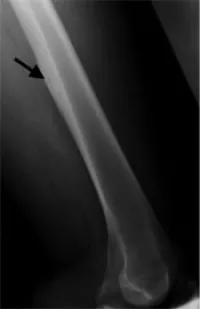
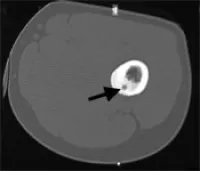
Imaging usually is very typical: X-rays show new bone formation and sometimes a small lucent spot (smaller than 1.5 cm), which is defined as the nidus. Computed tomography (cat scan, CT) is even better suited to show the new bone formation and the nidus. Because there may be a lot of inflammatory swelling and edema in the bone and soft tissues around the tumor magnetic resonance imaging (MRI) may sometimes be difficult to interpret and CT may be required to further assess these tumors. Radionuclide or bone scans show increased uptake of the radioactive tracer, this may sometimes be very focal.

Osteoid Osteoma Treatment
Osteoid osteoma is a benign tumor, it is not cancer, it does not spread to other regions of the body and does usually not increase in size. In rare instances this tumor even heals spontaneously. Therefore the tumor does not necessarily have to be removed.
Treating the pain
The most significant symptom of osteoid osteoma is pain, this can be treated with aspirin, ibuprofen or other over-the-counter anti-inflammatory drugs. Some patients have relief from certain medications for a while, but then these medications stop working. A change to another anti-inflammatory medication may then be required.
It should, however, be considered that stomach ulcers, heartburn and bleeding problems may develop from the use of anti-inflammatory medications.
Treating with operation
Surgical treatment has been the standard for a long time. However, for successful surgery the tumor must be completely removed. Sometimes these surgeries are quite extensive, require resection of large areas of bone and implantation of bone grafts. These have a higher risk of complications and a longer recovery period.
The operation usually entails a longer hospital stay of at least several days. Osteoid osteomas are frequently located in weight-bearing bones and during the recovery period from surgery a longer period of limited weight bearing is required, often with crutches for a number of weeks.
Treating minimal invasively with Radiofrequency Ablation (RFA):
Today the method of choice in many cases is radiofrequency ablation. During this procedure the tumor is heated up for a period of approximately 6 minutes and thus abladed. This procedure is minimal invasive, is done on an outpatient basis and has a short recovery time.
Since the nidus of an osteoid osteoma is usually very painful, the procedure is performed under general anesthesia.
The procedure can only be performed if the patient has the typical clinical and imaging findings. The location of the osteoid osteoma should permit a safe access and a safe heating/radiofrequency procedure without risking to damage nerves, major blood vessels and the skin. If the tumor nidus is more than 1 cm away from these structures the procedure can usually be safely performed.
The procedure takes approximately 2-3 hours including induction of general anesthesia. After the procedure the patient is taken to the recovery room and supervised by the anesthesiology team for approximately 4 hours. Patients then are able to leave the hospital with a prescription of pain medication.
The RF ablation is performed under sterile conditions in the CT suite to optimally localize the lesion. A thin biopsy needle, canula and drill needle are used to access the osteoid osteoma.
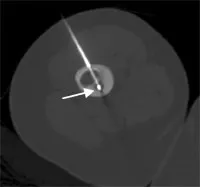
Then the drill is removed but the canula is left inside and the RF-probe is advanced through the canula into the nidus. The RF-probe is a straight rigid electrode with an outer diameter of 1 mm and it is insulated throughout its extent except the terminal 10 mm. The electrode is positioned in the center of the lesion to coagulate a sphere of tissue of 1cm diameter with the tip of the electrode at the center.
The electrode is connected to a radiofrequency generator. The electrode tip is heated up to 85-90 degrees Celsius for 6 minutes. Subsequently the probe and canula are withdrawn. There is usually no significant bleeding at the skin incision site and a bandage is sufficient to cover the puncture site.
On the day of the procedure patients will have pain and pain medication is required. In the following 72 hours pain will get better and after at least one week patients usually are free of pain. Within the first 48 hours patients usually will also be able to tell whether the typical tumor pain is gone.
Patients may return to work, school and other normal activities usually within the first week after the procedure. Please note, however, if the tumor is at a weight-bearing location (leg) sports, such as skiing, snowboarding, skate boarding, long distance running and jumping should be avoided for period of 3 months.
Two follow-up visits are recommended, one after one month, and a second after one year. These can be done by the patient’s doctor or orthopedist at home.
It should be considered that recurrence rates of 10-20% have been described and a second procedure may sometimes be required.
Treating non-invasively with High Intensity Focused Ultrasound (HIFU)
Get more information about High Intensity Focused Ultrasound.
Advantages of RF-ablation compared to surgery
- Rapid pain relief usually apparent within the first 2-3 days after the procedure,
- No overnight hospital stay,
- Return to work, school and other normal activities usually within the first week after the procedure, but no vigorous sports for 3 months,
- Minimal damage to bones and muscle with no significant structural weakness,
- Lower cost.
Assessing patients for treatment
In order to assess whether you qualify for this procedure we need to confirm your diagnosis of osteoid osteoma by reviewing the symptoms and the imaging studies. The CT scan is in particular important for this purpose, it will also help us to determine whether there is a safe needle access to the tumor without damage viable structures such as nerves, vessels and skin.
Prior to the intervention you will also need to be seen by our anesthesiologists in order to prepare for the anesthesia performed during the procedure.
A requirement for the procedure are also blood tests: parameters of the coagulation of the blood (PT, PTT, INR) as well as a complete blood count including thrombocytes. These blood tests are important to detect any abnormalities of blood clotting, which may be a risk for this procedure.

