T32 Radiology Fellows Share Their Experiences: Jae Ho Sohn, MD, MS and Evan Calabrese, MD, PhD
2. What was your primary T32 research project?
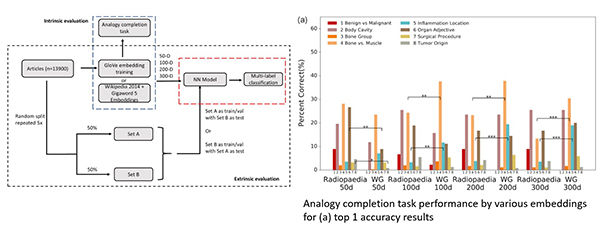
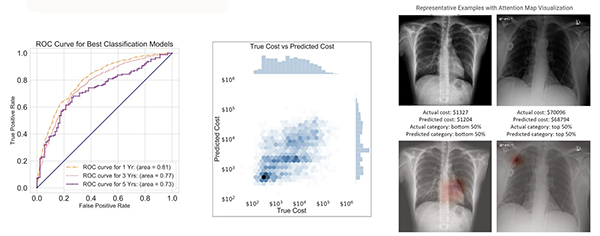
JHS: My research focused on big data in radiology (BDRAD). Specifically, I concentrated on two areas: radiological natural language processing (NLP) and computer vision in lung cancer screening CTs. NLP projects involved automatically extracting useful information from radiology reports, modeling radiological ontology, and providing imaging decision support. Lung cancer screening projects focused on nodule detection, characterization, and longitudinal registration as well as health imaging biomarker extraction from chest CTs.
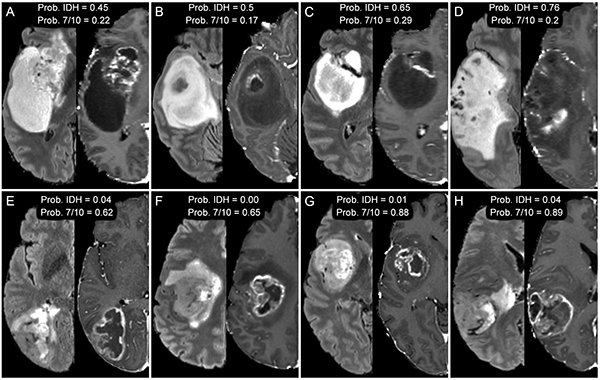
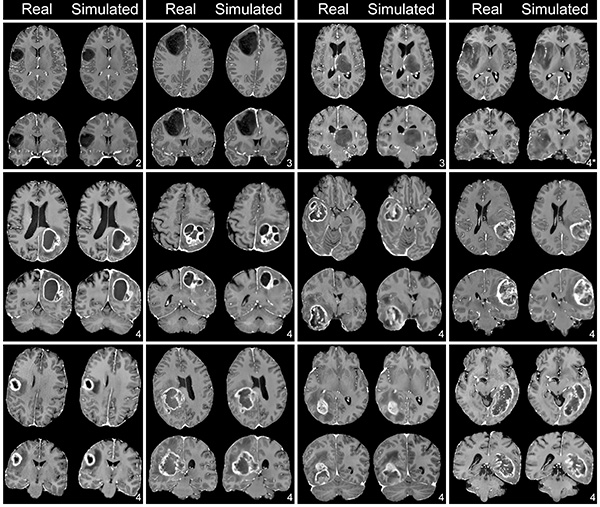
EC: My primary project is focused on predicting the presence of clinically relevant genetic biomarkers in glioblastoma using preoperative brain MRI. The idea is to use non-invasive imaging (rather than brain biopsy or resection) to determine important genetic characteristics of this aggressive form of brain cancer that can help guide treatment and inform prognosis.
3. How do you think the T32 program benefitted your career in academic radiology?
JHS: It was an important year that jumpstarted my research lab. A year of dedicated research helped me consolidate my research interests, create a collaborative network of researchers, recruit, and train key talents for the research lab, and build fundamental skills needed to succeed in my future academic career.
EC: The T32 program has given me an opportunity to do high level research during residency without compromising my clinical training. I think this will put me in a much better position to apply for early career faculty grants when I find an academic job that suits my interests.
4. How can your research translate into clinical setting to improve patient care?
JHS: My natural language processing projects apply broadly to both clinical and basic science aspects of radiology. A few practical examples include improving imaging decision support to ensure the best imaging protocol is chosen for a specific clinical indication while reducing errors in radiology report dictations. Similarly, computer vision projects focus on improving diagnostic accuracy of lung cancer screening and extracting useful health imaging biomarkers to improve the value of lung cancer screening. Long term, I hope to establish improved structured organization of cardiothoracic imaging and radiological text data so that my team and radiologist community at large can more easily discover hidden connections that exist within the data.
EC: Glioblastoma is the most common form of brain cancer and has a very poor prognosis. My project, if successful, could allow early recognition of different molecular subtypes of glioblastoma that can benefit from specific targeted therapies without the need for invasive biopsy or resection, which is not always possible or desirable for patients. I imagine my work and other work like it allowing us to non-invasively stratify patients into different prognosis groups and direct them towards the best therapy choice at the time of tumor diagnosis rather than weeks to months later when they can get a biopsy or tumor resection.
5. What are your plans after completing the T32 program?
JHS: I will be joining UCSF Radiology as a faculty member in Cardiac & Pulmonary Imaging and more formally launching a lab focusing on NLP and computer vision in cardiothoracic imaging. Additionally, I will work closely with the UCSF Center for Intelligent Imaging (Ci2) and other computational groups at UCSF, other UC campuses, and internationally.
EC: I hope to find a research path academic radiology position at a major U.S. academic medical center.
Dr. Calabrese, along with current T32 Trainees Milan Manchandia, MD and Tyler Gleason, MD, will present their year-long projects virtually on June 24 and June 25, 2021. Visit our events page for more information.
