Research Looks at the Predictive Value of Non-Contrast Head CT with Negative Findings in the Emergency Department Setting
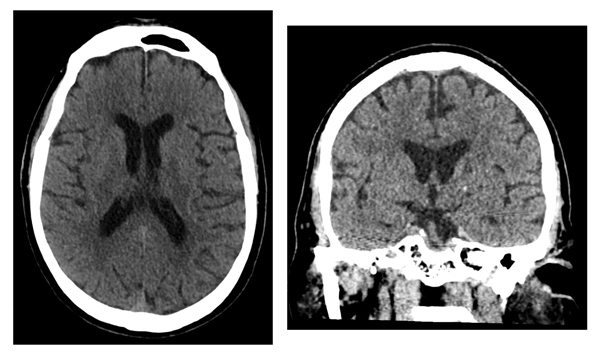
In the emergency department (ED), non-contrast head CTs are routinely acquired for patients with neurologic symptoms. Anecdotally, non-contrast head CTs performed in patients with prior negative findings on CTs performed for the same clinical indication are of low diagnostic yield. As such, a team of scientists led by the UC San Francisco Department of Radiology and Biomedical Imaging's Neuroradiology Section evaluated the rate of findings in patients who received serial head CTs in the emergency department. They hypothesized that the rate of acute findings in non-contrast head CTs performed in patients with a preceding negative study performed for a similar indication would be lower compared with patients being imaged for the first time or for a new indication. Findings were recently published in the American Journal of Neuroradiology (AJNR).
 "The paper shows that information readily available in the medical record can have significant impact on the 'predictive value' of an imaging study that a provider may be about to order," says Leo Sugrue, MD, PhD, the senior author and assistant professor in residence at UCSF Radiology.
"The paper shows that information readily available in the medical record can have significant impact on the 'predictive value' of an imaging study that a provider may be about to order," says Leo Sugrue, MD, PhD, the senior author and assistant professor in residence at UCSF Radiology.
To perform the research, scientists retrospectively analyzed approximately 10,000 CT scans performed in the ED setting over a four-year period. Scans show that a prior negative CT performed for a similar indication makes it much less likely that a new CT will have a clinically significant finding when compared to first-time examinations or examinations performed for a new indication. Results suggest that a prior negative head CT examination has a negative predictive value in terms of the likelihood that a new exam performed for the same clinical indication will be positive.
 "In medicine, we are all familiar with 'frequent fliers' to the ED. Our data suggests that when presenting with a similar clinical indication, repeat noncontrast head CTs are of limited diagnostic yield for this patient population," says Andrew Callen, MD, neuroradiology clinical fellow and first author on this study.
"In medicine, we are all familiar with 'frequent fliers' to the ED. Our data suggests that when presenting with a similar clinical indication, repeat noncontrast head CTs are of limited diagnostic yield for this patient population," says Andrew Callen, MD, neuroradiology clinical fellow and first author on this study.
"Such information could potentially be incorporated into decision support systems to reduce unnecessary imaging and its associated cost both in terms of money and radiation exposure," says Dr. Sugrue.
Christopher Hess, MD, PhD, UCSF Radiology chair, was also a contributing author on this study.
