Preventive imaging exams are designed to detect cancer and noncancerous health conditions in their early stages, when diseases are more treatable and curable. While physicians keep current with preventive care guidelines and recommend and encourage patients to have appropriate screenings, only a small portion of eligible patients receive recommended screenings. The consequences for individuals can be tragic and the costs to our community are significant. Primary care providers and gynecologists and those within the radiology community at UCSF Radiology are partners in advocacy, referring patients for screening and therefore improving survival rates.
Many are unaware that one of the key ways to prevent osteoporosis is to screen for it. At UCSF Radiology, we support recommendations by the National Osteoporosis Foundation that women age 65 and older and men age 70 and older undergo regular bone density screening tests. Beyond age, there are other risk factors which reduce the screening age to 40 years old for some candidates. These include race, body type and a number of lifestyle factors, ranging from exercise and diet to drinking and smoking. "Unfortunately, very few patients who meet expected criteria get screened for osteoporosis," says Thomas Link, MD, PhD, chief of Musculoskeletal Imaging. Dual-energy X-ray absorptiometry (DXA or DEXA) bone density scanning is recommended as the most accurate method available for the diagnosis of osteoporosis, as well as an accurate estimator of fracture risk. Those who test positively for low bone density should be screened every one to two years to ensure osteoporosis medication is working properly. Other options for measuring bone density include Quantitative Computed Tomography (QCT), invented here at UCSF.
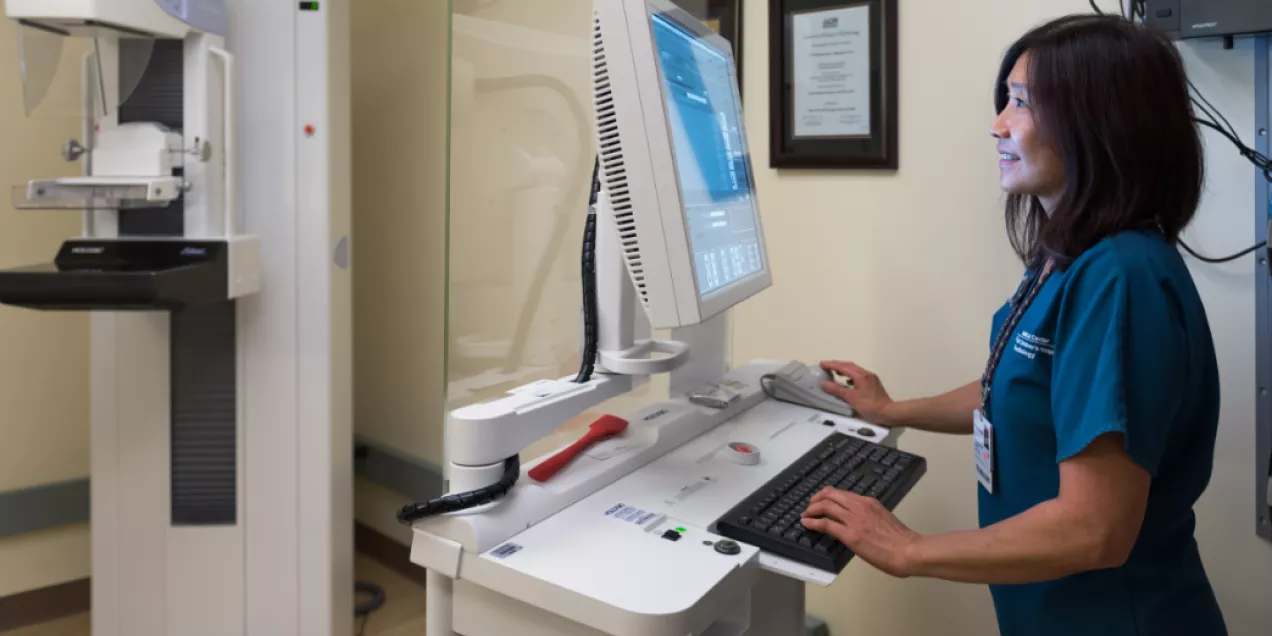
Despite highly controversial opposition from the U.S. Preventative ServicesTask Force, (USPSTF), UCSF Radiology stands with guidelines from the American College of Radiology, the National Comprehensive Cancer Network, the Society of Breast Imaging and additional health organizations that recommend annual breast cancer screening at age 40. Such recommendations are further supported by a recent landmark mammography study published in Cancer, the official journal of the American Cancer Society, which looked at mammography screening over 40 years. The study found that women who were screened lowered their mortality risk by 60 percent within 10 years and 47 percent within 20 years. According to the Centers for Disease Control and Prevention (CDC), 65.3 percent of women over age 40 received a mammogram within the past two years. "A combination of both screening and therapy are essential. Earlier screening leads to more effective therapy," says Bonnie Joe, MD, PhD, chief of Breast Imaging. UCSF Radiology's Breast Imaging Clinical Section provides expert mammography, breast ultrasound and breast MRI.
While colorectal cancer is the third-most commonly diagnosed cancer in the United States, a majority of cases can be prevented with proper screening. According to the American Society for Gastrointestinal Endoscopy (ASGE), half of adults who should have colonoscopies do not comply with recommended guidelines, while more than 60 percent of Americans age 50 and older have not used any method of colorectal cancer screening. Presently, the USPSTF recommends those with average risk for colorectal cancer begin screening at age 50; those with a family history are advised to start before then. However, the American Cancer Society (ACS) now recommends that people of average risk should start regular screening at age 45. The ACS says the incidence of colorectal cancer is declining in those age 50 and older, due to better screening rates. "While no one set of [colorectal cancer] screening guidelines is universally accepted at this time," says Ronald Zagoria, MD, chief of Abdominal Imaging, "primary care physicians should consider these new recommendations." UCSF Radiology offers virtual colonoscopy (VC) as a less invasive way to safely and effectively screen patients allowing for prevention, early detection and early intervention.
Lung cancer is the leading cause of cancer death in the United States. The USPSTF recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults age 55 to 80 who have a 30 pack-year smoking history. These guidelines apply to those who currently smoke or have quit within the past 15 years. However, according to an analysis done by the American Society of Clinical Oncology (ASCO), only 1.9 percent of 7 million current and former heavy smokers were screened for lung cancer in 2018. The study also found that just 1 percent of eligible smokers in the West received the recommended low-dose CT screening, the lowest rate of the four regions for which results were separated. Additionally, the USPTF recommends that screening takes place in centers, such as UCSF, with subspecialty level expertise in the diagnosis and treatment of lung cancer. The CT Lung Cancer Screening Program at UCSF Radiology uses radiology tools to detect lung cancer in at-risk patients at its earliest stages, when the disease is more treatable and curable. The International Association for the Study of Lung Cancer (IASLC) published its support of CT lung cancer screening based on the results of two large-scale studies, the National Lung Screening Trial (NLST) and the Dutch-Belgian Randomized Lung Cancer Screening (NELSON) trial. "As both these trials have pointed out, lung cancer survival rates are improved when CT lung cancer screening is used," says Brett Elicker, MD, chief of Cardiac and Pulmonary Imaging.
All orders from physicians outside UCSF start with a referral. Learn how to refer a patient.