Newly Published Research Reports an Important Discovery About Abdominal Aortic Aneurysms (AAAs)
Abdominal aortic aneurysm (AAA) disease is common; approximately 200,000 people in the U.S are diagnosed each year. They occur when the walls of the aorta bulge or dilate. If the aneurysm is intact, it will generally cause no health problems, however, larger AAAs can rupture, becoming life-threatening and requiring emergency surgery. Ruptured AAA is the 10th leading cause of death in men older than 55.
At present, clinical management of patients with asymptomatic AAA is determined primarily by the maximal aneurysm diameter. Patients with AAAs larger than 5.5 cm are normally referred for elective repair, whereas AAAs smaller than 5.5 cm are most commonly followed with serial imaging at 6-month to 3-year intervals, depending on their size. Ultrasound and cross-sectional imaging with CT or MRI are commonly used.
Scientists at the UC San Francisco Department of Radiology and Biomedical Imaging and the Veterans Administration Medical Center realized that this diameter-based management strategy has limitations as it does not factor in additional aneurysm features, including intraluminal thrombus (ILT), aneurysm wall inflammation, and biomechanical vessel wall stress that are also potential markers of rapid AAA growth and rupture.
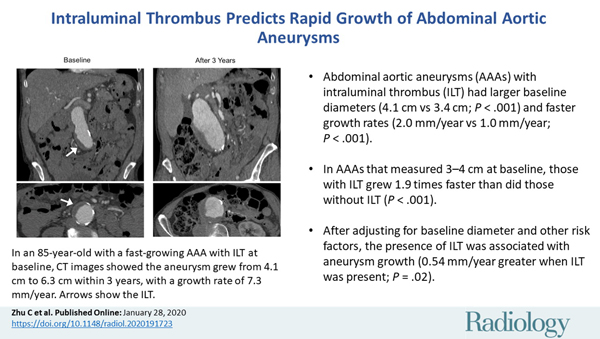
 Chengcheng Zhu, PhD and Joseph Leach, MD, PhD, first authors of the study, recently published in Radiology, focused on the intraluminal thrombus (ILT), a blood clot on the wall of the aorta at the location of the aneurysm. He and his colleagues noted that intraluminal thrombi are present in the majority of aneurysms close to the repair threshold of 5.5 cm, and also in a considerable number of smaller aneurysms. The influence of these clots on AAA growth and rupture risk, prior to the study, was not fully understood, and they sought out to see if ILT could be a new marker for aneurysm growth.
Chengcheng Zhu, PhD and Joseph Leach, MD, PhD, first authors of the study, recently published in Radiology, focused on the intraluminal thrombus (ILT), a blood clot on the wall of the aorta at the location of the aneurysm. He and his colleagues noted that intraluminal thrombi are present in the majority of aneurysms close to the repair threshold of 5.5 cm, and also in a considerable number of smaller aneurysms. The influence of these clots on AAA growth and rupture risk, prior to the study, was not fully understood, and they sought out to see if ILT could be a new marker for aneurysm growth.
To perform the study, they used high resolution cross-sectional imaging with CT or MRI to assess 225 male patients with AAA. Patients were from the SFVAMC. Follow-up lasted, on average, more than 3 years. A little over half of patients had an ILT. The aneurysms of those with ILT were larger at baseline and grew by a rate of 2 millimeters (mm) per year, twice as fast as the 1 mm per year growth rate in people without intraluminal thrombus.
 "An aneurysm with thrombus grows much faster than one without a thrombus," said Dr. Zhu in a statement to RSNA. "Our study looked at a large number of patients with a relatively long follow-up to confirm that thrombus is a new risk factor that may be potentially reported by radiologists."
"An aneurysm with thrombus grows much faster than one without a thrombus," said Dr. Zhu in a statement to RSNA. "Our study looked at a large number of patients with a relatively long follow-up to confirm that thrombus is a new risk factor that may be potentially reported by radiologists."
The overall findings of this study are significant because they suggest that imaging follow-up schedules may need adjustment for patients with AAA and a thrombus. At this time, protocols for follow-up imaging are based on the size of the aneurysm and do not account for the absence or presence of a thrombus.
"A patient at high risk may need closer monitoring," said Dr. Zhu. "If in patients with a thrombus the aneurysm grows twice as fast, then shortening the surveillance interval could be considered."
Further research is needed before thrombus detection is integrated into clinical protocols. At present, findings provide an additional piece of information for use in determining the prognosis of patients with this AAA.
Collaborating with Drs. Zhu and Leach were Yuting Wang, MD, Warren Gasper, MD, David Saloner, PhD and Michael Hope, MD. This was a retrospective study with patient data included from January 2004 through December 2018 at the San Francisco Veterans Affairs Health Care System (SFVAHCS). You can view materials, methodology and overall results in Radiology.
