Examining the Impact of Implicit AAA Screening on the Veteran Population
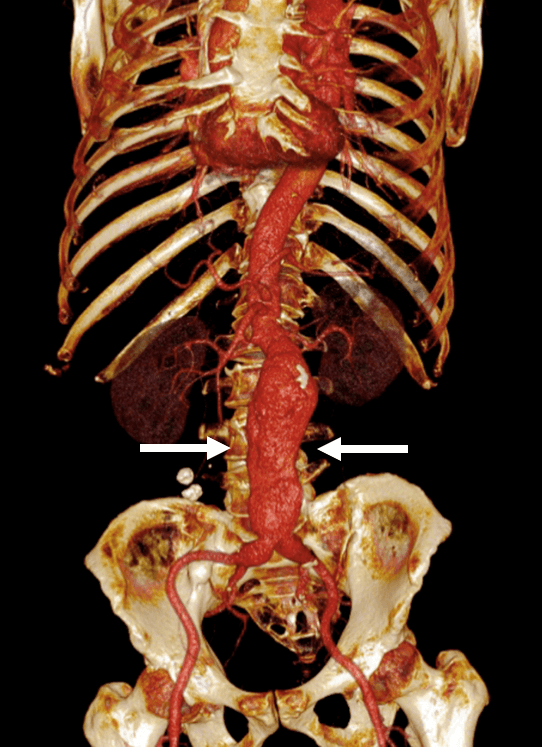 Abdominal aortic aneurysm (AAA) is a dilation or “bulging” of the abdominal segment of the aorta, the major artery that carries blood from the heart to the rest of the body. While most small AAAs are asymptomatic and pose little danger, larger AAAs have a risk of fatal rupture and are referred for surgical or endovascular repair to prevent this from occurring.
Abdominal aortic aneurysm (AAA) is a dilation or “bulging” of the abdominal segment of the aorta, the major artery that carries blood from the heart to the rest of the body. While most small AAAs are asymptomatic and pose little danger, larger AAAs have a risk of fatal rupture and are referred for surgical or endovascular repair to prevent this from occurring.
Because of this risk, AAA screening programs have been implemented in the U.S. and around the world to detect these aneurysms earlier at smaller diameters, allowing for surveillance and intervention to reduce rupture incidence. The US Preventative Services Task Force (USPSTF) recommends that men aged 65 to 75 years with any history of smoking undergo a one‐time AAA screening via ultrasonography.
“Since AAA screening programs have been put into effect, most studies have looked at implementation of these USPSTF recommendations at the institutional, local and regional level or on broader geographic scale in a narrower sense, but little attention has been paid to the significance of what we call ‘implicit AAA screening’,” says Joseph Leach, MD, PhD, assistant professor in residence in the Department of Radiology and Biomedical Imaging at UCSF. Implicit AAA screening can be defined as screening via any imaging study that evaluates abdominal aortic caliber. This includes radiology examinations performed for a range of abdominal indications, e.g., a computed tomography (CT) scan of the abdomen and pelvis performed to evaluate diffuse abdominal pain.
Dr. Leach maintains an active research program at UCSF and the San Francisco Veterans Affairs Medical Center (SFVAMC). His research goal is to improve characterization of vascular diseases and to identify risk factors for serious outcomes, such as the AAA rupture. He recently received a VA CDA-2 Grant, a major Career Development Award within the VA System.
 Dr. Leach was part of a team of UCSF faculty based at the VAMC that examined the association between imaging‐based AAA screening - both explicit and implicit - and various outcomes for approximately 1.6 million veterans in the VA health system over ten years (from 2005 to 2015). Their findings were recently published in JAHA, the journal of the American Heart Association. Team members included Dimitrios Mitsouras, PhD, Eugene Huo, MD, Thomas Hope, MD and Michael D. Hope (former faculty). Mary Whooley, MD, professor, and Hui Shen, statistician, both from the UCSF School of Medicine, were also key contributors to this study.
Dr. Leach was part of a team of UCSF faculty based at the VAMC that examined the association between imaging‐based AAA screening - both explicit and implicit - and various outcomes for approximately 1.6 million veterans in the VA health system over ten years (from 2005 to 2015). Their findings were recently published in JAHA, the journal of the American Heart Association. Team members included Dimitrios Mitsouras, PhD, Eugene Huo, MD, Thomas Hope, MD and Michael D. Hope (former faculty). Mary Whooley, MD, professor, and Hui Shen, statistician, both from the UCSF School of Medicine, were also key contributors to this study.
“Implicit AAA screening reflects the common post hoc screening practices of providers in a wide diversity of clinical settings and is an often overlooked but key adjunct to explicit screening examinations targeting fulfillment of the USPSTF screening recommendation,” say the team of researchers.
This study was a retrospective observational analysis of the association between AAA screening, via explicit and implicit mechanisms, and various outcomes, including mortality in the veteran population. “Our data suggests that although AAA screening in the VA population is only moderately successful in terms of reach, it is substantially greater than other analyses have suggested because of consideration of implicit screening,” say the investigators. They note that careful accounting for and use of implicit screening data can likely have a greater impact than expansion of formal explicit screening on all-cause mortality and AAA rupture on the population scale.
Such work is part of one of the team’s research goals to meaningfully advance the assessment of AAA risk in patients who do not meet current intervention thresholds and improve outcomes by refining surveillance imaging regimens and decisions regarding early intervention for AAAs.
