Improving Workflow and Care Delivery for Stroke Patients

According to Christopher Hess, MD, PhD, professor and chair of the UC San Francisco Department of Radiology and Biomedical Imaging, speed in treatment is critical for patients suffering from a stroke. It can make a difference between successful recovery, permanent disability or even death. UCSF Radiology works on improving workflow and efficient care delivery for better stroke diagnosis and more impactful treatment. This includes MRI and angiography suites such as the ones located at Zuckerberg San Francisco General Hospital (ZSFG), the only Level 1 Trauma Center in San Francisco and a Joint Commission-certified Stroke Center.
"The benefit of having these multimodality angiography suites is that we're able to decide in real time how to process with embolectomy," says Dr. Hess. "Our technology advantage is also bolstered by additional imaging resources including cone-beam CT, effective hub-and-spoke imaging transfer tools and fast emergency department CT. Having these tools helps make sure patients do not hemorrhage before an embolectomy."
Improving workflows also means allowing patients to avoid going through the ER, putting them directly into the hands of UCSF neurointerventional radiologists who can start procedures right away, since we know that time is very important when treating stroke patients.
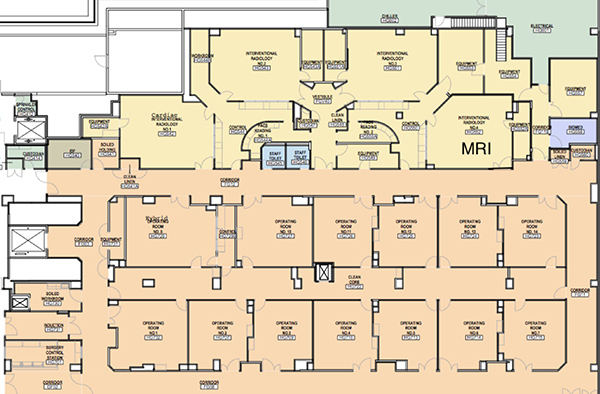
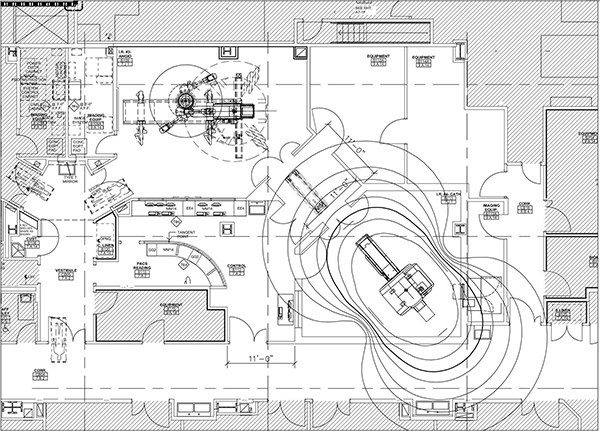
"Our facilities at ZSFG are equipped to treat acute stroke with combined a biplane X-ray angiography suite and a 3T MRI scanner in a common procedural space in the operating room. This enables us to diagnosis and provide therapy in a single location, leading to better stroke outcomes," says Mark Wilson, MD, professor in residence at UCSF Radiology and chief of Radiology at ZSFG.
"We designed the combined X-ray angiography and 3T MRI suite at ZSFG to be the best stroke treatment suite in the world. We can navigate catheters under the best X-ray imaging and gather physiologic information about the brain with MRI," shares Steven Hetts, MD, professor and chief of interventional neuroradiology at UCSF Mission Bay Hospitals. "This has improved our intra-procedure and post-procedure decision-making, in support of providing the best care to stroke patients."
Additionally, this technology helps with the timeliness of thrombolysis, performed using tissue plasminogen activate (tPA) in patients with large-vessel occlusion. With this procedure, the tPA protein, used to dissolve the clot, must be given intravenously within a four-and-a-half-hour window from onset of symptoms, ensuring treatment success. Timeliness also comes into play to a lesser extent for endovascular therapy, a procedure performed by neuroradiologists with the goal of removing a clot in the brain. Imaging plays a key role in selecting patients for embolectomy procedures.
This example is one that demonstrates the importance and potential future of multimodality imaging. Such improvements highlight one of ZSFG's many goals to provide emergency medicine to underserved populations along with extensive stroke research programs designed to improve care for stroke patients.
Portions on this blog are based on an article that appeared on Healthcare-in-Europe.com.
