Breast Imaging Study Supports Targeted US as the Primary Imaging Modality for the Evaluation of Palpable Lumps in Lactating Women
Women today are increasingly delaying childbirth into their 30s and 40s. The National Center for Health Statistics (NCHS) says that 18.3 percent of births were to mothers of advanced maternal age (35 and over) in 2018. The New York Times reports that first-time mothers are older in big cities and on the coasts, including in the Bay Area where the average age hovers around 31. This trend in delayed childbirth means that more women are lactating into their 30s and 40s, when mammography would typically be the initial imaging modality to evaluate palpable masses in the general population. A palpable breast mass is the most common manifesting symptom of breast cancer.
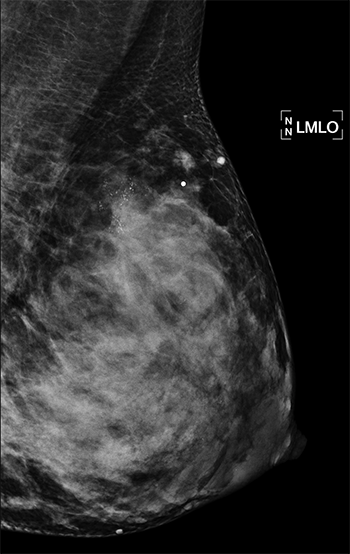
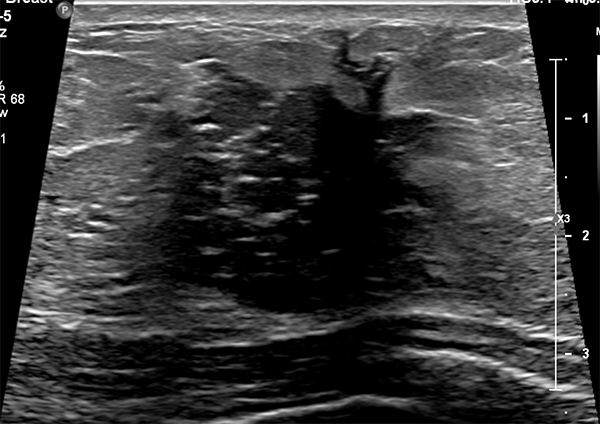 Breast imaging during pregnancy and lactation is already challenging due to both physiologic and structural changes to the breast. In addition, the American College of Radiology (ACR) reports that “Pregnancy-associated breast cancer (PABC) is increasing as more women delay child bearing into the fourth decade of life, and imaging of clinical symptoms should not be delayed.” At this time, guidelines from the American College of Radiology (ACR) recommend ultrasound as the first-line imaging modality for the evaluation of palpable masses in pregnant and lactating women, but data regarding breastfeeding women age 30 years and older are near nonexistent.
Breast imaging during pregnancy and lactation is already challenging due to both physiologic and structural changes to the breast. In addition, the American College of Radiology (ACR) reports that “Pregnancy-associated breast cancer (PABC) is increasing as more women delay child bearing into the fourth decade of life, and imaging of clinical symptoms should not be delayed.” At this time, guidelines from the American College of Radiology (ACR) recommend ultrasound as the first-line imaging modality for the evaluation of palpable masses in pregnant and lactating women, but data regarding breastfeeding women age 30 years and older are near nonexistent.
 With this in mind, a team of breast imaging radiologists from the UC San Francisco Department of Radiology and Biomedical Imaging and the Mayo Clinic Department of Radiology set out to evaluate the diagnostic performance of targeted ultrasound as the primary imaging modality for the evaluation of palpable masses in lactating women, including those of advanced maternal age. Their second aim was to evaluate the added benefit of mammography.
With this in mind, a team of breast imaging radiologists from the UC San Francisco Department of Radiology and Biomedical Imaging and the Mayo Clinic Department of Radiology set out to evaluate the diagnostic performance of targeted ultrasound as the primary imaging modality for the evaluation of palpable masses in lactating women, including those of advanced maternal age. Their second aim was to evaluate the added benefit of mammography.
Co-authors analyzed data from 167 symptomatic, breastfeeding women—at an average age of 35—who underwent targeted ultrasound. They found that ultrasound scored high marks, sensitivity and specificity of 100 percent and 70 percent respectively. Positive predictive value of an abnormal examination and positive predictive value of biopsy were 9.4 percent and 10 percent, respectively. In those who underwent mammography in addition to US, mammography added seven false-positive findings without additional cancer diagnoses. Specificity was lowered with the addition of mammography from 67 percent to 61 percent. These results support US as the primary modality for the evaluation of palpable lumps in breastfeeding women. You can read the full methodology of this study, which is the largest to date, in Radiology.
Corresponding author on this study was Amie Lee, MD, associate professor in the Breast Imaging section at UCSF Radiology. Lead author on this study was Maggie Chung, MD, PGY4 radiology resident. Additional authors from UCSF Radiology include Jessica Hayward, MD, Heather Greenwood, MD, Kimberly Ray, MD, faculty in the breast imaging section and Bonnie Joe, MD, PhD, chief of breast imaging.
“It is important to point out that mammography is still our primary diagnostic imaging tool for lumps in general,” says Dr. Joe. “This paper addressed a very specific scenario of breastfeeding women at an average age of 35.” Bilateral mammography should be considered in women age 40 years or older if screening mammography has not been performed within the last year. Mammography should also be performed in all women with highly suspected or known breast cancer.
For more information about screening for breast cancer, please read this previous blog post.
