Using Applied Statistics for a Practical Diagnostic Framework for Negative COVID-19 Results
 Uncertainty around diagnostic testing for the coronavirus has been a dilemma for clinicians throughout the COVID-19 pandemic. Due to low reported sensitivities for molecular testing, CT evaluation of persons under investigation (PUIs) has become more popular as a supplement to RT-PCR testing. A common occurrence is for a PUI to repeatedly test negative for COVID-19 yet their chest CT imaging findings are consistent with COVID-19. When this is the case, what does the treating team do?
Uncertainty around diagnostic testing for the coronavirus has been a dilemma for clinicians throughout the COVID-19 pandemic. Due to low reported sensitivities for molecular testing, CT evaluation of persons under investigation (PUIs) has become more popular as a supplement to RT-PCR testing. A common occurrence is for a PUI to repeatedly test negative for COVID-19 yet their chest CT imaging findings are consistent with COVID-19. When this is the case, what does the treating team do?
In order to address this dilemma, a team of physicians from the UC San Francisco Department of Radiology and Biomedical Imaging and the San Francisco Veterans Affairs Medical Center (SF VAMC) have worked on and presented a framework for how to weigh repeatedly negative test results in clinical decision making when there is ongoing concern for COVID-19.
In order to display provide this framework, they presented a case and covered the applied clinical statistics to address how many serial RT-PCR tests are needed to effectively rule out COVID-19 infection. The full case review and framework was recently published and are available for review in Respiratory Medicine Case Reports (Open Access).
“It is very easy to anchor to a diagnosis in the setting of the ongoing COVID-19 pandemic,” says Masis Isikbay, MD, PGY3 resident and lead author on this study. “It is for this reason we hope the applied statistics in this case will give providers a practical framework for contextualizing multiple negative RT-PCR tests for various patient populations.”
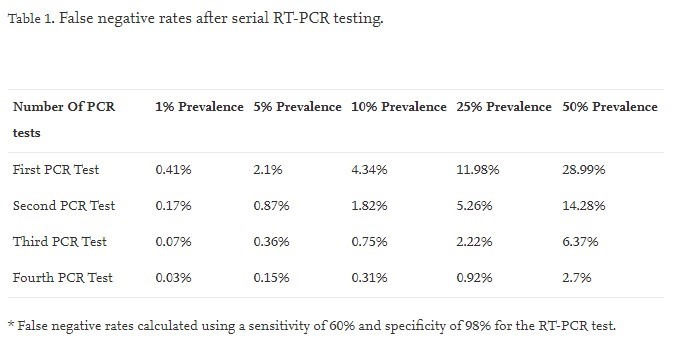
Overall, COVID-19 infection should be effectively ruled out with three negative RT-PCR results. In areas of higher disease burden (prevalence of 25%), the false negative rate after four RT-PCR tests is below 1%. Even with a very high prevalence of 50%, the false negative rate is low (2.7%) after four negative tests, suggesting that alternative diagnoses should be strongly considered. See the table below for more information.
Travis Henry, MD, former acting chief of Cardiac and Pulmonary Imaging at UCSF Radiology, Michael Hope, MD UCSF Radiology faculty and chief of radiology at the SF VAMC, and James Frank, MD, professor, co-director of the ICU and attending physician at the SF VAMC were also authors on this work.
