Parkinson’s disease and Deep Brain Stimulation
 Melanie Morrison, PhD, is an assistant professor in residence in the Department of Radiology and Biomedical Imaging at UCSF, and a core member of the UCSF-UC Berkeley Joint PhD Program in Bioengineering. With her team in the new Neuromodulation Lab, she researches imaging techniques with the potential to treat the symptoms of Parkinson’s disease.
Melanie Morrison, PhD, is an assistant professor in residence in the Department of Radiology and Biomedical Imaging at UCSF, and a core member of the UCSF-UC Berkeley Joint PhD Program in Bioengineering. With her team in the new Neuromodulation Lab, she researches imaging techniques with the potential to treat the symptoms of Parkinson’s disease.
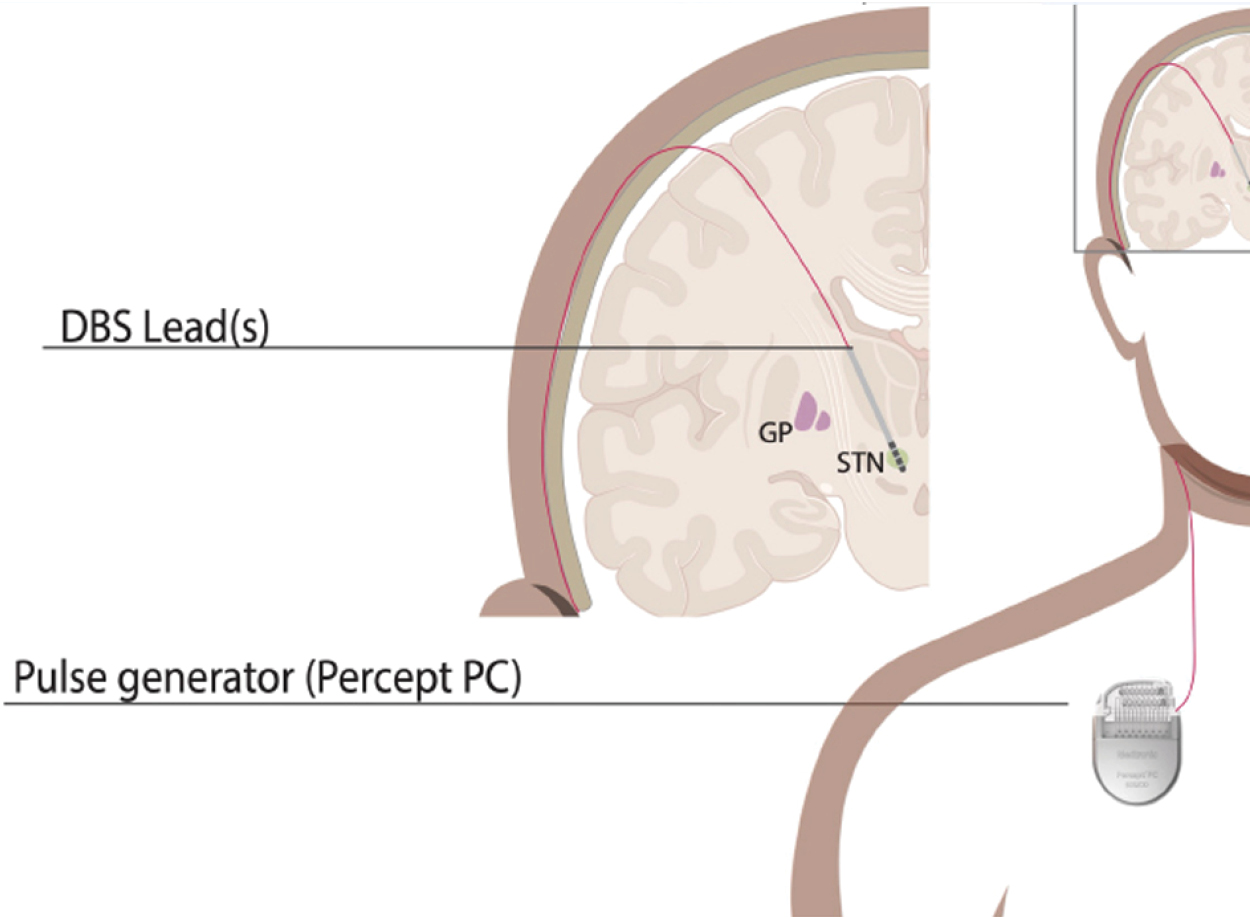
Dr. Morrison and her collaborators use MRI and other advanced imaging techniques to improve neuromodulation therapies for patients with neuropsychiatric conditions such as Parkinson’s disease and obsessive-compulsive disorder (OCD). This neuromodulation technique, called Deep Brain Stimulation (DBS), uses an implant that delivers electrical current to targeted brain areas to restore function. Dr. Morrison and her colleagues extract quantitative information from brain MRI images to study and predict patients’ neural and clinical responses to DBS.
DBS was first approved for Parkinson’s treatment in 2002, and there are currently around 200,000 patients worldwide with DBS implants. During the initial procedure, the surgeon places a neurostimulator, a small, battery-operated device, under the skin near the collarbone. This device is connected to electrodes in the brain via wires that run under the skin. The neurostimulator sends electrical impulses to the targeted areas of the brain, which can help to reduce the symptoms of various neurological disorders such as Parkinson’s and OCD.
DBS implants help patients achieve greater stability through the day than medication alone, as the medication levels in their bloodstream vary with natural biological cycles. As Dr. Morrison described it, “DBS is a second line therapy. Patients see a lot of fluctuations in their daily medication cycle, inconsistencies in the medication levels. It doesn’t mean the medication stops working, it’s just less effective as Parkinson’s progresses. DBS helps when they would otherwise feel their motor symptoms come back more frequently throughout the day.”
This therapy has seen great success, but there remains a need to address variability in patient outcomes and the bottleneck to wider implementation arising from limited number of multidisciplinary clinical teams of neuropsychologists, neurologists, neurosurgeons who conduct DBS procedures and provide patient follow up.
Fortunately, there are many potential ways to use MRI to improve patient outcomes and streamline the therapy. As Dr. Morrison describes it, “The automated tools we are currently aiming to develop will help identify the best candidates, and the optimal parameters and settings for the medical device to personalize it to the individual. We are looking for ways to streamline all parts of the implementation from pre-operative candidate selection and surgical planning all the way through post-op optimization of therapeutic device setting.”
Dr. Morrison observed that “The lab is at the beginning of what I hope is going to be a pretty exciting research program. We are developing new tools and imaging techniques for studying different populations that benefit from DBS. Our team includes neurologists and neurosurgeons, as well as neuroscientists and psychiatrists to support us, along with our network of collaborators, and we all work in a very close level of connectivity. This is very in-person, collaborative research, in an exciting growing field.“
To learn more, please visit the Neuromodulation Lab.
