Imaging Scientists Advance Prostate Cancer Research

September is Prostate Cancer Awareness Month and the Department of Radiology and Biomedical Imaging is at the forefront of research to understand prostate cancer and develop treatments. These are just a few of the publications this year by our researchers.
Research Highlights
Whole-Body Diffusion-Weighted Imaging Spots PSMA-negative Lesions
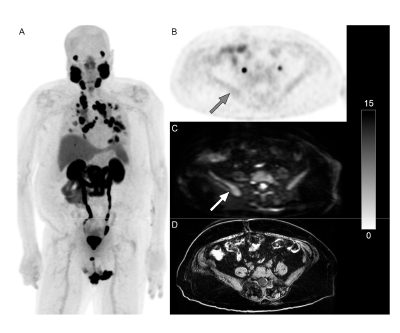 Adding whole-body diffusion-weighted imaging (WB DWI) to PSMA PET scans for patients with metastatic castration-resistant prostate cancer can allow radiologists to identify PSMA-negative lesions, potentially altering their treatment plan. The most common locations for these lesions were the lymph nodes followed by bones and, less frequently, the lungs and liver.
Adding whole-body diffusion-weighted imaging (WB DWI) to PSMA PET scans for patients with metastatic castration-resistant prostate cancer can allow radiologists to identify PSMA-negative lesions, potentially altering their treatment plan. The most common locations for these lesions were the lymph nodes followed by bones and, less frequently, the lungs and liver.
This research was published in the Journal of Clinical Medicine in March 2025.
Authors: Cheng William Hong, Spencer Behr, Fei Jiang, Yingbing Wang, Sina Houshmand, Thomas Hope
Nanocarriers Predict Drug Delivery to Prostate Tumors
 A team of UCSF researchers created two different nanocarriers labeled with a radioactive marker to track their movement in various prostate tumors, measuring the enhanced permeability and retention effect. Using PET scans they found that some prostate cancer tumors have low and uneven nanocarrier uptake and penetration, likely due to irregular blood vessel development. These new nanocarriers can be used to predict drug delivery and efficacy, helping doctors personalize treatment by identifying which tumors are most likely to be affected by this therapy.
A team of UCSF researchers created two different nanocarriers labeled with a radioactive marker to track their movement in various prostate tumors, measuring the enhanced permeability and retention effect. Using PET scans they found that some prostate cancer tumors have low and uneven nanocarrier uptake and penetration, likely due to irregular blood vessel development. These new nanocarriers can be used to predict drug delivery and efficacy, helping doctors personalize treatment by identifying which tumors are most likely to be affected by this therapy.
The study was published in Molecular Cancer Therapeutics in January 2025.
Authors: Niranjan Meher, Anil Bidkar, Anju Wadhwa, Kondapa Naidu Bobba, Suchi Dhrona, Chandrashekhar Dasari, Changhua Mu, Cyril Fong, Juan A. Cámara, Umama Ali, Megha Basak, David Bulkley, Veronica Steri, Jun Zhu, Adam Oskowitz, Rahul R. Aggarwal, Renuka Sriram, Jonathan Chou, David Wilson, Youngho Seo, Daniel V. Santi, Henry VanBrocklin, Robert Flavell. For all authors see the paper.
Deep Learning Automates Tumor Measurement in MRI
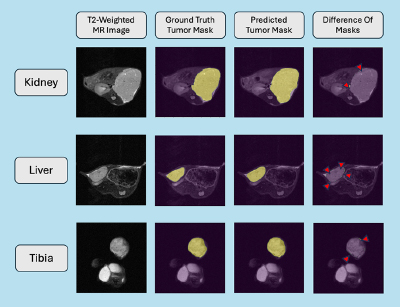 A new deep learning method paired with MRI can automatically measure tumor size. Demonstrated in mice, in this two-step process a classifier identifies which MRI slices show tumor, then a segmentation model outlines the tumor on those slices. The top-performing model in the test batch, a dense recurrent residual U-Net, was highly accurate. This automated system works for other tumor sites like kidneys, liver, and tibia, and can save time and improve accuracy for cancer research.
A new deep learning method paired with MRI can automatically measure tumor size. Demonstrated in mice, in this two-step process a classifier identifies which MRI slices show tumor, then a segmentation model outlines the tumor on those slices. The top-performing model in the test batch, a dense recurrent residual U-Net, was highly accurate. This automated system works for other tumor sites like kidneys, liver, and tibia, and can save time and improve accuracy for cancer research.
The study was published in Tomography in February 2025.
Authors: Satvik Nayak, Henry Salkever, Ernesto Diaz, Avantika Sinha, Nikhil Deveshwar, Madeline Hess, Matthew Gibbons, Sule Sahin, Abhejit Rajagopal, Peder Larson, Renuka Sriram
Using Multivariate Hyperpolarized C13 MRI to Predict Prostate Cancer Outcomes
 The standard predictive measures of prostate cancer outcome are based on histology, size, location and other clinical measures. However, these are often not accurate necessitating improved methods for detecting aggressive, clinically-significant prostate cancers. In prior studies, hyperpolarized C13 pyruvate MRI, using pyruvate-to-lactate conversion rates to measure cellular metabolism, showed the ability to detect aggressive cancers in the prostate and their response to therapy. In this study of metastatic prostate cancers, a new multivariate framework enabled prediction of time-to-progression and overall patient survival with high statistical accuracy. This new multivariate framework extracted 316 features from metabolic maps to more accurately gauge the metabolic aggressiveness of these advanced cancers. These features were used to develop risk classifiers for patient outcomes, as a less aggressive metabolism is correlated with a better prognosis. The researchers’ multi-feature risk classifier called the Metabolic Prognostic Score (MPS) has the potential to become powerful, non-invasive prognostic biomarkers for advanced prostate cancer.
The standard predictive measures of prostate cancer outcome are based on histology, size, location and other clinical measures. However, these are often not accurate necessitating improved methods for detecting aggressive, clinically-significant prostate cancers. In prior studies, hyperpolarized C13 pyruvate MRI, using pyruvate-to-lactate conversion rates to measure cellular metabolism, showed the ability to detect aggressive cancers in the prostate and their response to therapy. In this study of metastatic prostate cancers, a new multivariate framework enabled prediction of time-to-progression and overall patient survival with high statistical accuracy. This new multivariate framework extracted 316 features from metabolic maps to more accurately gauge the metabolic aggressiveness of these advanced cancers. These features were used to develop risk classifiers for patient outcomes, as a less aggressive metabolism is correlated with a better prognosis. The researchers’ multi-feature risk classifier called the Metabolic Prognostic Score (MPS) has the potential to become powerful, non-invasive prognostic biomarkers for advanced prostate cancer.
This work was published in Cancers in July 2025.
Authors: Hsin-Yu Chen, Ivan de Kouchkovsky, Robert Bok, Michael A. Ohliger, Jane Wang, Daniel Gebrezgiabhier, Tanner Nickles, Lucas Carvajal, Jeremy W. Gordon, Peder Larson, John Kurhanewicz, Rahul Aggarwal, Daniel Vigneron
Identifying Cancer Cell Percentages in Prostate Lesions with Multiparametric MRI
 It is common for prostate cancer lesions to be mixtures of cancer with benign tissues. This study evaluated this characteristic and the ability of MRI to detect such lesions. Over a third of the cancer lesions in this study contained mostly benign tissue. These tend to be small and not very aggressive. When they present with a mostly cancerous core and a mostly benign periphery, they tend to be larger and more aggressive, while lesions that are mostly cancer tend to be even larger and more aggressive. Although more difficult to see on MRI, these lesions that are mostly benign tissue can still often be detected with MRI, particularly when they present with a mostly cancerous core. This may prove valuable for focal treatment planning to capture the cancer lesion fully. Lesions that contained some aggressive cancer but still mainly benign tissue could not be differentiated from non-aggressive cancers that had little benign content, which could lead to underreporting and undertreating some cancers. Based on this study, these aggressive cancers mixed with primarily benign tissue were rare.
It is common for prostate cancer lesions to be mixtures of cancer with benign tissues. This study evaluated this characteristic and the ability of MRI to detect such lesions. Over a third of the cancer lesions in this study contained mostly benign tissue. These tend to be small and not very aggressive. When they present with a mostly cancerous core and a mostly benign periphery, they tend to be larger and more aggressive, while lesions that are mostly cancer tend to be even larger and more aggressive. Although more difficult to see on MRI, these lesions that are mostly benign tissue can still often be detected with MRI, particularly when they present with a mostly cancerous core. This may prove valuable for focal treatment planning to capture the cancer lesion fully. Lesions that contained some aggressive cancer but still mainly benign tissue could not be differentiated from non-aggressive cancers that had little benign content, which could lead to underreporting and undertreating some cancers. Based on this study, these aggressive cancers mixed with primarily benign tissue were rare.
The study was published in Magnetic Resonance Imaging in December 2024.
Authors: Olga Starobinets, Jeffry P. Simko, Matthew Gibbons, John Kurhanewicz, Peter R. Carroll, Susan Noworolski
