After Lung Cancer Treatment, Radiation Pneumonitis Can Mimic Tumor Growth
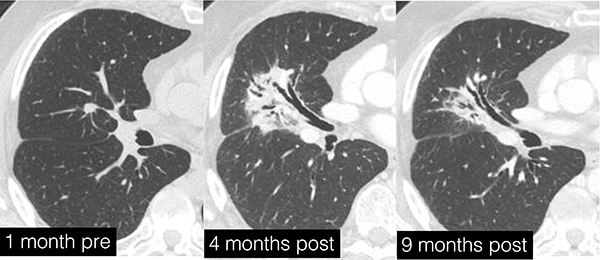
The treatment for lung cancer with the “Cyber Knife” (thoracic stereotactic body radiation therapy) went well, but six months later the patient notices something wrong with her breathing, and a new round of imaging shows a growing mass at the tumor site. Instead of cancer recurrence, close examination of the new imaging studies show that the mass is acute radiation pneumonitis, characterized by acutely inflamed tissue around the treatment site.

Kimberly Kallianos, MD, presented her findings on oncologic therapy-induced lung disease at the RSNA 2024 annual meeting. She explained that acute radiation pneumonitis and the associated chronic fibrosis in the lungs can manifest six to 12 months after SBRT treatment and can evolve for about one year. This condition, though distressing, can often be resolved or improved with steroid treatment.
This diagnosis is often challenging, as sometimes radiation pneumonitis or fibrosis can appear in the lungs even when a patient has not had prior treatment for lung cancer. After radiation therapy for head and neck cancer or breast cancer, lung tissue may still respond to off-target radiation damage with inflammation that looks like new lung cancer or metastasized tumors.
Pulmonary parenchymal effects can also appear in response to drug toxicity; immunotherapy for lung cancer produces high rates of pneumonitis, which generally appears around two to four months after treatment begins. Even mild existing interstitial lung disease increases odds of this reaction. Clinicians are often alarmed by the change in lung scans, especially in sensitive, immune-suppressed patients, as it can mimic new cancer signs. However, withdrawing the drug which caused the reaction, accompanied by steroid treatment, can resolve many manifestations of pulmonary, drug toxicity. There are concerns around resuming drug treatment after the fibrosis, as 50% of patients have a second reaction after the drug is resumed, but in the meantime the patient will breathe easier.
Radiation, though a great tool in fighting cancer, can cause secondary tissue damage. Understanding the potential signs of these after-effects can save patients and referring clinicians the stress and anxiety of fearing a cancer recurrence and reduce the chance of overtreatment.
