Vascular Birthmarks: Creating Order from a Palette of Red, Purple, and Blue
The patient with a vascular birthmark presents a challenge to the physician, as many entities that may look alike carry different diagnoses and are treated far differently. A vascular birthmark is distinct from other types of birthmarks, such as a pigmented birthmark. Thus, a big brown spot is not the same as a big spot that is red, purple or blue.
Vascular birthmarks can be partitioned into two groups, based on clinical and cellular characteristics. One group is tumors that involve blood vessel elements. The other group is vascular malformations, which involve the blood vessel elements themselves.
Vascular malformations consist of a group of lesions comprised of malformed blood vessel elements. They can involve arteries, veins, capillaries, lymphatics, or a combination thereof. A port wine stain, for example, is a capillary malformation.
Vascular malformations are present at birth, whether or not they are identified at birth, as they represent alterations in blood vessel development in utero. While some vascular malformations are not discovered until adulthood, we are treating many childhood birthmarks and growths at UCSF. With the new UCSF Benioff Children's Hospital set to open in 2015, this is particularly relevant. History, physical examination, and imaging will facilitate an accurate diagnosis in most
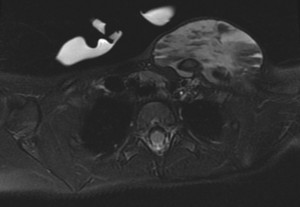
Almost everybody who has a vascular malformation will need imaging of some sort to evaluate it. Imaging helps us to know what structures are involved and how deep the lesion is. It could be what we call a “tip of the iceberg” lesion where only a little bit is visible on the skin surface but it goes deeper and involves muscles, bone or something else. Imaging, which is almost always magnetic resonance imaging (MRI), allows us to look at the lesion in question and understand how it relates to the other tissues. Other modalities are effective, too, such as computed tomography (CT) when bones are involved, angiography when blood vessels are involved, and ultrasound for other situations.
Many vascular malformations can be treated by minimally invasive radiological techniques, including sclerotherapy (for lymphatic and venous malformations) and transarterial embolization (for arteriovenous malformations.) In some cases, surgery, medical management, or no therapy may be optimal, depending on tissue type, symptoms, and anatomic location.
In conjunction with Ilona Frieden MD, of UCSF’s Birthmark and Vascular Anomaly Center (BVAC), I will be discussing the role of Interventional Neuroradiology in treating vascular anomalies at an upcoming Grand Rounds on December 10, 2013.
The BVAC was established in 1991 and serves as a valuable regional, national, and international resource for physicians and patients who are dealing with confusing vascular lesions. Dr. Frieden, an internationally-recognized pediatric dermatologist, founded the BVAC and serves as its director. I am pleased to collaborate with Dr. Frieden at the Center, where I am a co-director along with William Hoffman, MD from the Division of Plastic and Reconstructive Surgery at UCSF. The Center is fortunate to have Neuroradiologist Christopher Hess, MD, PhD, an expert in the imaging of vascular birthmarks, as a participating physician.
In the continuum of medicine, pediatric dermatology and neurointerventional radiology could not be farther apart, so it is might seem odd for two such different specialties to be working closely together like we do at the BVAC. However, the collaboration is a very practical application, which is yielding wonderful results for patients.