TURP Alternatives: What Urologists Need to Know About Prostate Artery Embolization (PAE)
 Benign prostatic hyperplasia (BPH), also known as prostatic enlargement, is a common condition in aging men. BPH often causes lower urinary tract symptoms (LUTS), which can result in poor quality of life.
Benign prostatic hyperplasia (BPH), also known as prostatic enlargement, is a common condition in aging men. BPH often causes lower urinary tract symptoms (LUTS), which can result in poor quality of life.
Transurethral resection of prostate (TURP) is one of several surgical therapies used to treat BPH, and while it is currently considered the gold standard for BPH treatment, it requires general anesthesia and a longer recovery period. Sexual side effects are common.
Prostate artery embolization (PAE) is performed by interventional radiologists as part of a class of procedures called minimally invasive image-guided procedures (MIIPs). Inclusion criteria for PAE candidates include:
- Patients with severe LUTS due to BPH, including an International Prostate Symptom Score (IPSS) score of 20 or more or American Urological Association Symptom Index (AUA-SI) QoL score of 4 or more.
- Prostate size minimum of 40g.
- Patients who have failed medical management including insufficient improvement with medical therapy or intolerance to medical therapy.
There are exclusion criteria to consider before offering patients PAE. These include renal failure, uncorrectable coagulopathy, severe atherosclerosis/vessel tortuosity and confounding disease of lower urinary tract. These are all considered during initial consultation.
According to Ryan Kohlbrenner, MD, assistant professor in the Interventional Radiology subspecialty in the UC San Francisco Department of Radiology and Biomedical Imaging, there is considerable overlap between TURP candidates and PAE candidates. He feels as though interventional radiologists at UCSF Radiology can help urologists the most with the following patient demographics:
- Patients who are not surgical candidates, either because they are unable to tolerate general anesthesia or because their prostates are too big.
- Patients who do not want a transurethral procedure, or are afraid of impotence, incontinence, or retrograde ejaculation. These are far more common after TURP.
- Patients with hematuria of prostatic origin.
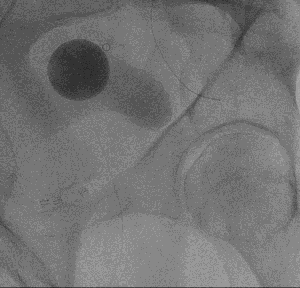
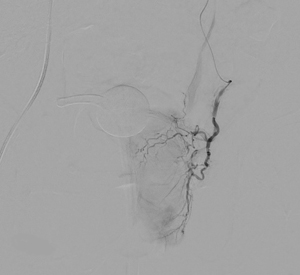 Overall, the procedure involves shrinking the prostate by treating its blood vessels. An interventional radiologist gains access through a small incision in the upper thigh or the wrist. From there, small particles are injected into the prostate to slow the blood flow to the gland, causing the prostate to shrink. Relief from BPH symptoms occurs in the following weeks and months. It is a relatively painless procedure using conscious sedation. After the procedure, UCSF Radiology follows up with patients at one, six and 12 months.
Overall, the procedure involves shrinking the prostate by treating its blood vessels. An interventional radiologist gains access through a small incision in the upper thigh or the wrist. From there, small particles are injected into the prostate to slow the blood flow to the gland, causing the prostate to shrink. Relief from BPH symptoms occurs in the following weeks and months. It is a relatively painless procedure using conscious sedation. After the procedure, UCSF Radiology follows up with patients at one, six and 12 months.
There is lots of current evidence to support the safety and efficacy of PAE. Some of the most well-known are listed below:
- Recent Meta-Analyses
- Recent Prospective Trials
- Recent Subgroup Studies
For additional information on PAE as a TURP alternative, and a deeper dive into current evidence supporting PAE, hear directly from Dr. Kohlbrenner by watching a video of his lecture.
