Nuclear Medicine Week Research Roundup
We celebrate Nuclear Medicine Week during the first full week of October. It is an opportunity to learn more about nuclear medicine techniques, their benefits, and how they are used to diagnose and treat various medical conditions, as well as to feature the researchers and medical professionals who make it happen.
UCSF Radiology and Biomedical Imaging clinicians and researchers are applying nuclear medicine to diagnose and treat illnesses including cancer. These are just a few of their recent accomplishments in research and clinical trials.
Recent Accomplishments in Research and Clinical Trials
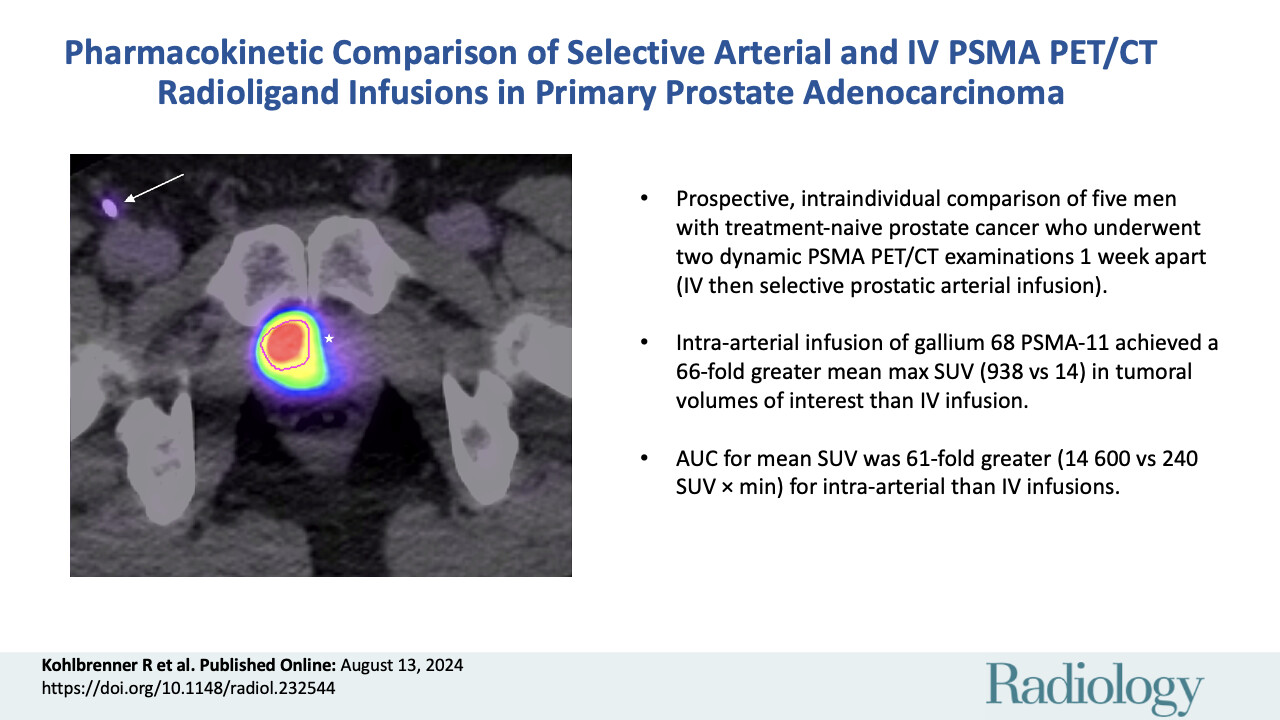
Should PSMA be Administered Through Arteries or Veins?
In Pharmacokinetic Comparison of Selective Prostatic Arterial and Intravenous PSMA PET/CT Radioligand Infusions in Primary Prostatic Adenocarcinoma, published in Radiology, researchers with the UCSF Department of Radiology and Biomedical Imaging and the Departments of Pathology and Urology compared intravenous and prostatic arterial infusions of the radiotracer through either the right or left prostatic artery. The study concluded that selective prostatic arterial infusion resulted in greater tumoral uptake than intravenous infusion.
First author Ryan Kohlbrenner, MD, Xiao Wu, MD, and senior author Tom Hope, MD, with their UCSF collaborators, explored this selective prostatic arterial administration on primary tumor uptake for intravenous prostate-specific membrane antigen (PSMA)-targeted radioligand therapy.
Kohlbrenner explained, "Our proof-of-concept study indicates that intra-arterial delivery of small amounts of a PSMA-based agent may enhance radioligand uptake in prostate cancer cells compared to intravenous injections, provided the disease is localized within a specific arterial distribution."
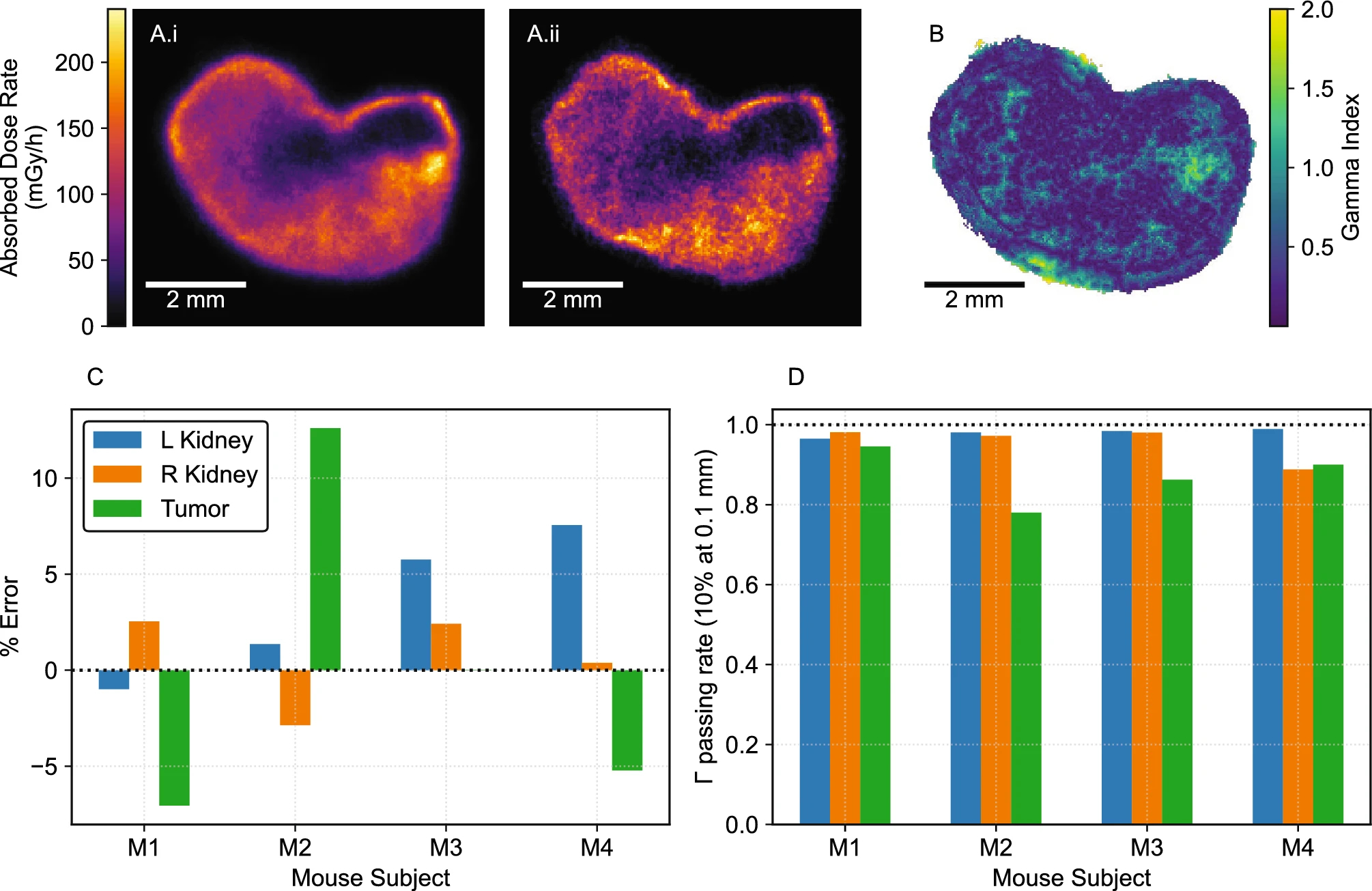
Measuring Where Radiopharmaceuticals Concentrate with Digital Autoradiography
3D small-scale dosimetry and tumor control of 225Ac radiopharmaceuticals for prostate cancer, published in Scientific Reports, explores methods of measuring the spatial dose distribution of radiopharmacuticals in organs and tumors, to inform treatment dose prescription and reduce off-target toxicity.
First authors Robin Peter and Anil Bidkar, PhD, with Kondapa Naidu Bobba, PhD, Luann Zerefa, Niranjan Meher, PhD, Anju Wadhwa, PhD, Rob Flavell, MD, PhD, and co-senior author Youngho Seo, PhD, joined colleagues from UC Berkeley and University of Arizona to investigate development of a 3D digital autoradiography (DAR) method to measure the spatial dose distribution of α-emitting radiopharmaceuticals. This allowed the research team to evaluate the effectiveness and toxicity of a novel therapeutic radiopharmaceutical for prostate cancer.
Seo said, “Small-, approaching even micro-, scale absorbed dose calculation can explain how alpha-emitting radiopharmaceuticals specifically target active areas in tumors.”
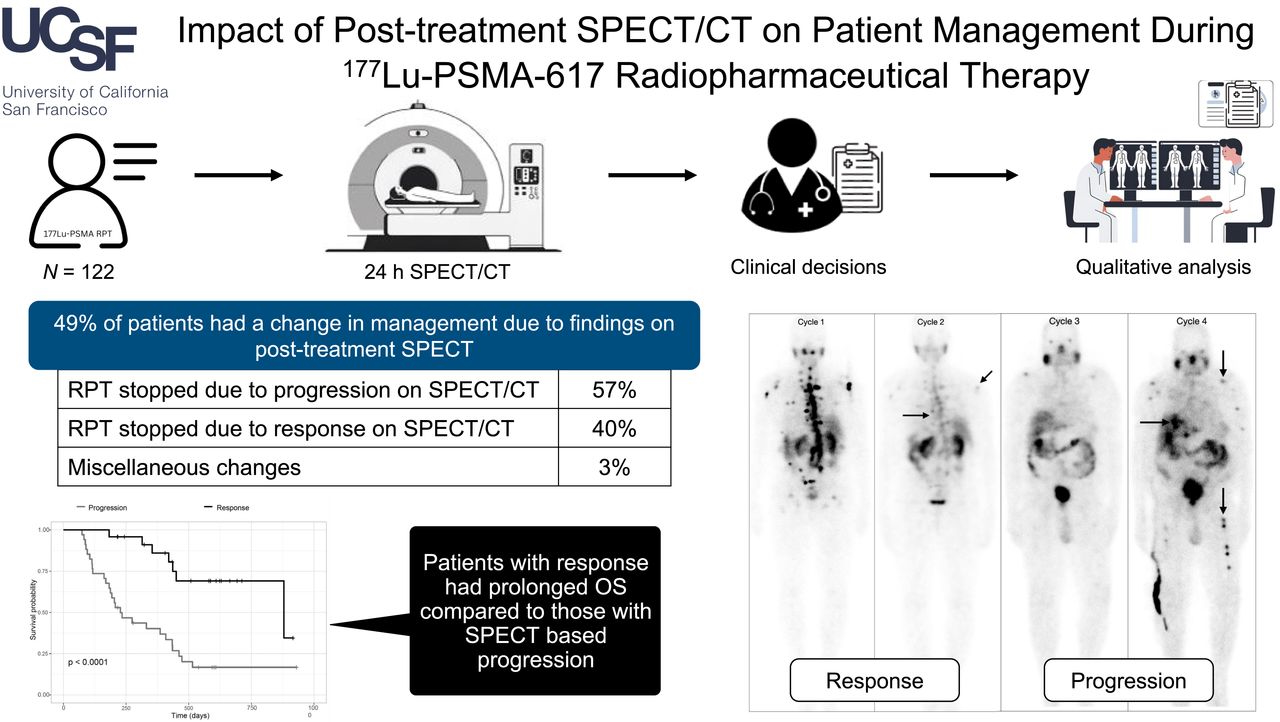
How often does post-treatment SPECT/CT impact patient management during Radiopharmaceutical Prostate Cancer Treatment
Impact of Posttreatment SPECT/CT on Patient Management During 177Lu-PSMA-617 Radiopharmaceutical Therapy, published in Journal of Nuclear Medicine, the study revealed that nearly 50% of patients experienced a change in management based on posttreatment SPECT/CT. In 28% of cases, disease progression was detected, leading to treatment discontinuation, while 20% showed response leading to treatment pauses. This is a cost-effective imaging approach to closely monitor disease progression with each radiopharmaceutical therapy (RPT) cycle.
The research was published by first author Surekha Yadav, MD, with Blair Lowrey, MD, Abuzar Moradi Tuchayi, MD, Rachelle Saelee, Roxanna Juarez, MD, Rob Flavell, MD, PhD, and senior author Tom Hope, MD.
Yadav emphasizes the potential impact on patient care, “Integrating posttreatment SPECT/CT into the routine PSMA RPT workflow can streamline personalized patient management by serving as a response marker to RPT.’’
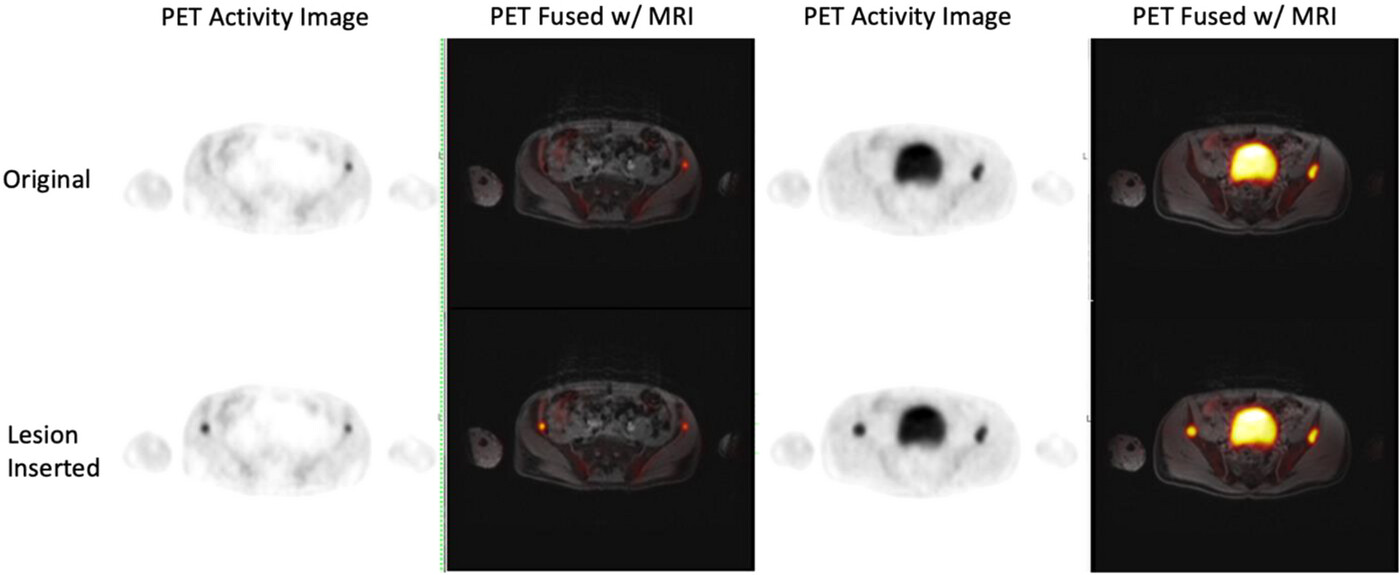
Improving PET/MR Cancer Imaging
Assessment of lesion insertion tool in pelvis PET/MR data with applications to attenuation correction method development, published in the Journal of Applied Clinical Medical Physics, explored training PET image correction tools with simulated cancer lesions to improve image quality of pelvis scans. The researchers evaluated different PET attenuation correction methods using a synthetic lesion digital tool that simulates lesions in images from patients. Pre-existing lesion images were simulated in a similar environment to where they were found, then synthetic lesions were included. The researchers found that the lesion insertion tool can simulate radiopharmaceutical uptake in pelvic lesions and their expected SUV values, and that the lesion insertion tool can be extended to evaluate further PET reconstruction corrections and algorithms and their impact on quantitation accuracy and precision.
Abhejit Rajagopal, PhD, Peder Larson, PhD, and Tom Hope, MD, joined authors from University of Southern California, Washington University in St. Louis, University of Washington, University of Utah, and GE Healthcare and iSono Health on this project.
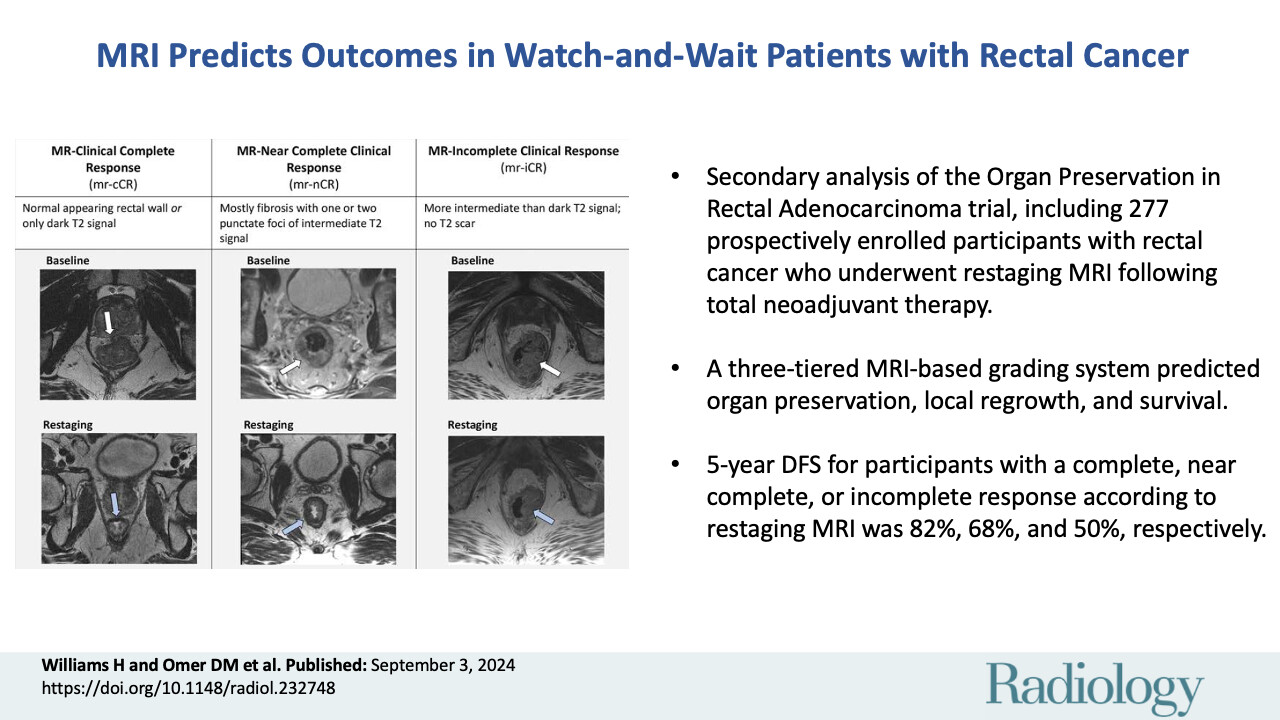
MRI Can Find When to Treat and When to Wait
MRI Predicts Residual Disease and Outcomes in Watch-and-Wait Patients with Rectal Cancer, published in Radiology, details a clinical trial explored MRI’s potential in assessing the best type of treatment for patients with rectal cancer. The team evaluated the ability of background MRI to accurately select rectal cancer patients for nonoperative management, predicting oncologic outcomes and identify imaging features associated with residual disease after total neoadjuvant therapy. They found that restricted diffusion and abnormal nodal morphologic features on restaging MRI scans were associated with increased likelihood of residual tumor.
Tom Hope, MD, was a member of the OPRA Consortium, which included 35 equally contributing authors from 15 universities and health systems.