A Less Invasive, Less Expensive Treatment for Spinal CSF-Venous Fistulas
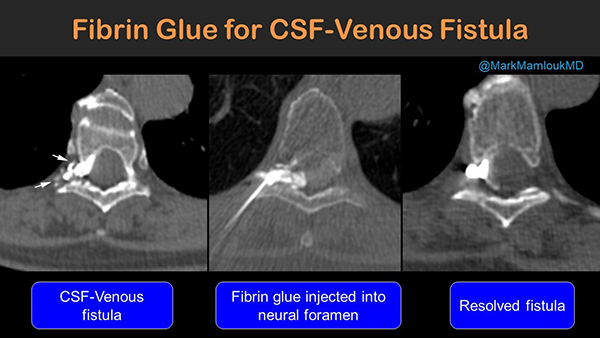
Spinal CSF-venous fistulas are one type of spinal leak and a cause of spontaneous intracranial hypotension (SIH). Patients with SIH represent a difficult diagnostic and therapeutic challenge requiring multiple complementary imaging modalities and disciplines. They are most commonly treated with open surgical ligation and have reportedly not responded well to percutaneous treatments. A team of neuroradiology and neurosurgery scientists set out to study treatment outcomes of CT-guided fibrin glue occlusion for patients with cerebrospinal fluid–venous fistulas (CVFs).
 Mark Mamlouk, MD, neuroradiologist at the Kaiser Permanente Santa Clara Medical Center and volunteer assistant clinical professor at the UC San Francisco Department of Radiology and Biomedical Imaging was corresponding author. He was joined by Kaiser Permanente colleagues Peter Shen, MD (former UCSF neuroradiology fellow) and Mark Sedrak, MD and William Dillon, MD, Elizabeth A. Guillaumin Professor of Radiology at UCSF Radiology. Their paper was recently published in Radiology.
Mark Mamlouk, MD, neuroradiologist at the Kaiser Permanente Santa Clara Medical Center and volunteer assistant clinical professor at the UC San Francisco Department of Radiology and Biomedical Imaging was corresponding author. He was joined by Kaiser Permanente colleagues Peter Shen, MD (former UCSF neuroradiology fellow) and Mark Sedrak, MD and William Dillon, MD, Elizabeth A. Guillaumin Professor of Radiology at UCSF Radiology. Their paper was recently published in Radiology.
The team conducted a retrospective review of medical records from two institutions for all patients with CVFs who underwent CT-guided percutaneous fibrin glue occlusion from March to October 2020. The CVFs were assessed for resolution or persistence at posttreatment decubitus CT myelography (CTM). They reviewed pre- and posttreatment brain MRI scans for principal signs of SIH. They documented clinical symptoms before and immediately after therapy, and the current symptoms to date after fibrin glue occlusion were documented. Of the 13 patients that received CT-guided fibrin glue occlusion, all showed improvement on post-treatment brain MRI scans.
 “In this paper, we showed that percutaneous fibrin glue injections can be an effective treatment for spinal CSF-venous fistulas,” says Dr. Mamlouk. “Previously, these fistulas were treated with neurosurgery and were only performed at a few centers across the U.S. Our new technique is less invasive, has a shorter recovery, is an outpatient procedure and is less expensive.”
“In this paper, we showed that percutaneous fibrin glue injections can be an effective treatment for spinal CSF-venous fistulas,” says Dr. Mamlouk. “Previously, these fistulas were treated with neurosurgery and were only performed at a few centers across the U.S. Our new technique is less invasive, has a shorter recovery, is an outpatient procedure and is less expensive.”
The authors note that further studies are needed to determine the long-term efficacy of this treatment.
