The Exploration of PSMA PET as a Possible Theranostic Agent in Thyroid Cancer
In the U.S., thyroid cancer is a common endocrine malignancy with about 52,890 new cases per year, according to the American Cancer Society. Most patients see a favorable response to surgery and risk-adapted postoperative therapy with thyroid hormone suppression and radioactive iodine (RAI) therapy, with external beam radiation therapy added in select high-risk situations. However, there is a subset of patients with aggressive and less-differentiated thyroid cancer resistant to RAI therapy, and unfortunately, these patients ultimately succumb to their illness. Treatment options are limited and their overall prognosis is poor.
Scientists at UC San Francisco identified an unmet clinical need for improved therapies for patients with aggressive forms of thyroid cancer that do not respond to RAI therapy. Right now, agents targeting prostate-specific membrane antigen (PSMA) are under investigation for both imaging and therapy of prostate cancer. In fact, UCSF and UCLA have recently obtained U.S. FDA approval for 68Ga-PSMA-11, the first PSMA radiotracer approved. But despite the name, PSMA expression is not specific to prostate, and is seen in a variety of normal tissues and cancers, including thyroid cancer.
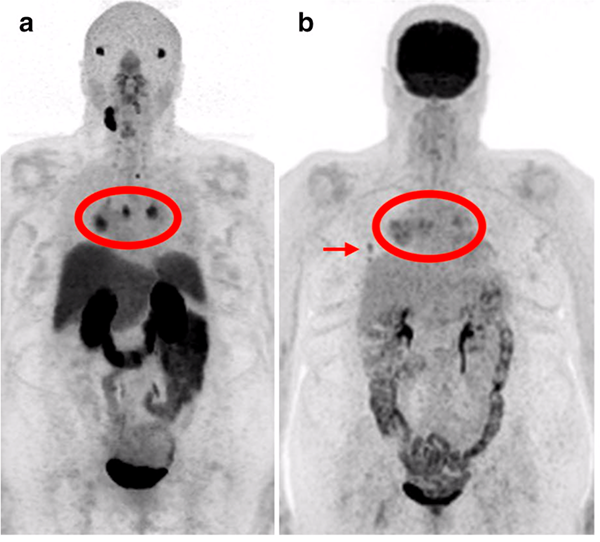
 Courtney Lawhn Heath, MD, assistant professor in the Molecular Imaging & Therapeutics clinical section at UCSF Radiology took the lead on a recent prospective pilot study, published in EJNMMI Research, to determine the feasibility and utility of [68Ga]Ga-PSMA-11 PET/MRI in thyroid cancer patients. The team of scientists enrolled eligible patients (adults with a history of pathology-proven thyroid cancer who had abnormal radiotracer uptake on recent 2-[18F]FDG PET and/or 131I). Patients underwent a [68Ga]Ga-PSMA-11 PET/MRI, and comparison was made to the prior qualifying 2-[18F]FDG PET CT/MRI for lesion location and relative intensity.
Courtney Lawhn Heath, MD, assistant professor in the Molecular Imaging & Therapeutics clinical section at UCSF Radiology took the lead on a recent prospective pilot study, published in EJNMMI Research, to determine the feasibility and utility of [68Ga]Ga-PSMA-11 PET/MRI in thyroid cancer patients. The team of scientists enrolled eligible patients (adults with a history of pathology-proven thyroid cancer who had abnormal radiotracer uptake on recent 2-[18F]FDG PET and/or 131I). Patients underwent a [68Ga]Ga-PSMA-11 PET/MRI, and comparison was made to the prior qualifying 2-[18F]FDG PET CT/MRI for lesion location and relative intensity.
"The exploration of PSMA PET as a possible theranostic agent in thyroid cancer is in its infancy," note the authors of the study. Overall, 68Ga-PSMA-11 demonstrated lower detection rate when compared to 2-[18F]FDG PET for thyroid cancer lesion visualization. They concluded that thyroid cancer subtype alone may not be sufficient to predict PSMA uptake, and radiotracer uptake may vary between patients and even within patients. Additionally, the authors note that future studies should include a larger number of patients, including dedifferentiated thyroid cancer subtypes, and should involve administration of PSMA radioligand therapy.
"Like other non-prostate cancers, PSMA-PET seems to have potential application in some, but not all patients," says Robert Flavell, MD, PhD, chief of Molecular Imaging and Therapeutics Clinical Section at UCSF Radiology and corresponding author on this study.
Sue Yom, MD, PhD, professor and radiation oncologist from the UCSF Departments of Radiation Oncology & Otolaryngology-Head and Neck Surgery also helped lead this study. Authors from UCSF Radiology include faculty members Javier Villanueva-Meyer, MD, Roxanna Juarez, MD, Spencer Behr, MD, Miguel Hernandez Pampaloni, MD, Christine Glastonbury, MBBS and Thomas Hope, MD and Maya Aslam (clinical research supervisor) and Raven Smith (clinical research coordinator). Jason Chan, MD (assistant professor) and Manpreet Narwal (senior clinical research coordinator) from Radiation Oncology and Chienying Liu, MD (UCSF Department of Medicine) also contributed.
