Pulsatile Tinnitus (PT) is a symptom that affects nearly five million Americans. The sensation of hearing a rhythmic noise, such as a heartbeat, swooshing or whooshing, from no external source, is, at best, a little unsettling; for many, the near constant sound exceeds annoyance and becomes completely debilitating. Nearly 60% of patients who experience this issue also suffer from some form of depression or anxiety. These rates are significantly higher than those associated with other chronic conditions due in large part to the difficulty of diagnosing the root cause of symptoms.
Common Causes of Pulsatile Tinnitus
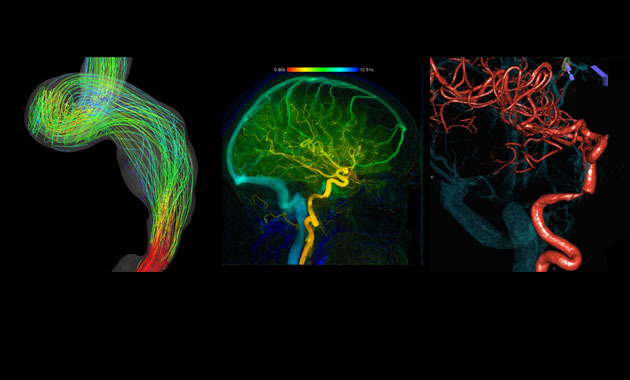
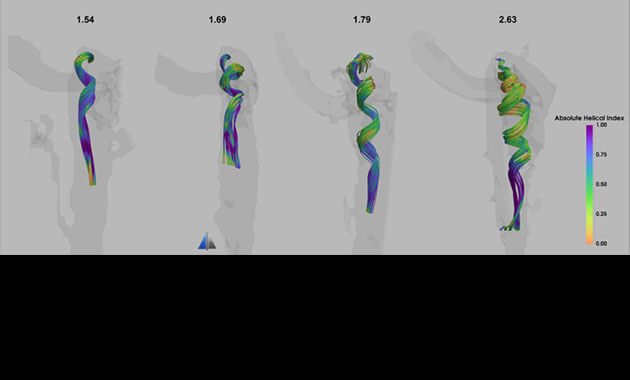
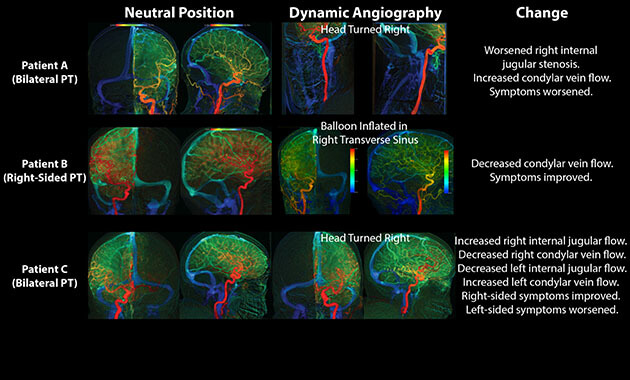
Pulsatile Tinnitus can have many different origins, some fairly benign, others potentially life-threatening. Sources can include vascular malformations, abnormal cerebral pressures, and unique blood flow patterns near the ear. The condition can also be caused by the presence of a tumor. Even when the causes of Pulsatile Tinnitus are fairly benign, its effects are sufficiently incapacitating for most patients to seek help.
Why Choose Pulsatile Tinnitus Treatment at UCSF
- Multidisciplinary approach involving specialists from the departments of Radiology, Neurology, and Psychiatry who collaborate to diagnose and treat this condition
- Strong reputation for resolution despite previous misdiagnosis
- Active research of Pulsatile Tinnitus to help future patients and outcomes
- Diagnosis success rate of over 90%
- Read One Patient’s Quest to End Ominous Ringing in Her Ear
Diagnosing Pulsatile Tinnitus
Physicians Referrals
For physicians seeking consultation or referrals, please contact us at (415) 502-3895
Please provide us with the following: PTC Referral Checklist (pdf)
- Referral from your physician
- Medical records including any pertinent notes regarding your symptoms and imaging reports
- Brain/Head/Neck Imaging (CT, MRI/A, PET, etc.), if any, copied to a CD
- Patient and insurance demographics (address, contact number and front and back copies of insurance cards)
- Insurance authorization for CPT codes: 99205 (evaluation) x2 units
When required, it is your responsibility to work with your referring physician to obtain prior authorization to your appointment. If your insurance does not require prior authorization please send a note with (call reference number, agent name, phone number, and message). If you have Medicare Part B, we do not need prior authorization.
- Please mail or fax to:
UCSF Pulsatile Tinnitus Clinic
505 Parnassus Ave. L308
San Francisco, CA 94143
Ph: (415) 502-3895
Fx: (415) 502-4017
- Once all information is received, the referral is carefully reviewed by our team to determine the most appropriate evaluation. Our office will contact patient or family directly within 2-4 weeks for scheduling.
Patients Self-Referrals
Patients can self-refer through the UCSF’s Second Opinion portal (please specify "Dr. Matthew Amans" to review). This is often preferred by those who:
- Seek a second opinion;
- Have not yet scheduled an appointment with a doctor regarding this condition.
Schedule a Virtual Consultation
About the Second Opinion program:
- A review of your case by Dr. Amans, who will communicate his 2nd opinion to you through UCSF’s Second Opinion portal. He will indicate whether he recommends the option to see him in clinic.
How does it work:
- Through the portal, please specify "Dr. Matthew Amans" to review.
- You will be asked for all relevant information for Dr. Amans to assist with your consultation.
- This includes your demographics, a description of your symptoms, and any prior images.
- With this information, Dr. Amans will be able to reach out to you directly to provide a rapid response to your question regarding your condition next steps. To access the portal, please visit: UCSF’s Second Opinion portal.
Highlights:
Convenience of PT diagnosis up front, without the need of scheduling an in-person meeting
- Determine if you have Pulsitile Tinnitus and what to do about it.
- Direct contact with world-leader in the field of Pulsitile Tinnitus.
- Quick turn around time.
- No need to schedule an in-person appointment for first consultation (diagnosis).
Pulsatile Tinnitus Treatments
Conditions Treated:
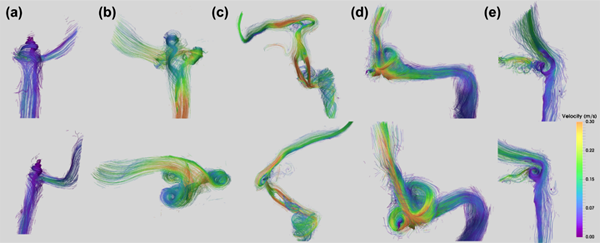
- Dural Arteriovenous Fistula (DAVF): Dural arteriovenous fistula is an abnormal connection between arteries and veins in the head. These can be dangerous and often require treatment by a neurointerventional radiologist using minimally-invasive image-guided catheter-based procedures. UCSF has pioneered many of the treatments for this condition.
- Carotid Stenosis: Carotid stenosis is an abnormal narrowing of an artery in the neck that carries blood to the brain. This can be dangerous and often requires treatment with medicines or procedures or both to relieve the narrowing. UCSF offers the full range of treatments for this condition, which may include medicines, image-guided procedures, surgical procedures, or a combination of these.
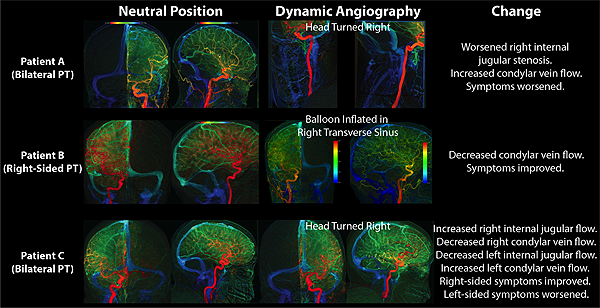
- Idiopathic Intracranial Hypertension (IIH): Idiopathic intracranial hypertension results in high pressures in the fluid (CSF) surrounding the brain, which causes headaches and high pressure in the eyes. This is usually first treated with weight loss and medicines. However, some patients need to be treated with procedures, such as stenting to improve blood flow out of the head, or other procedures to remove fluid from the head or cause weight loss.
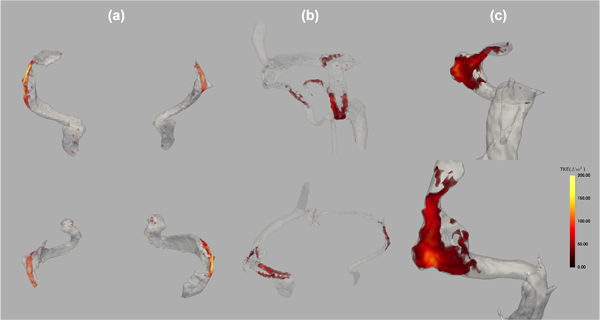
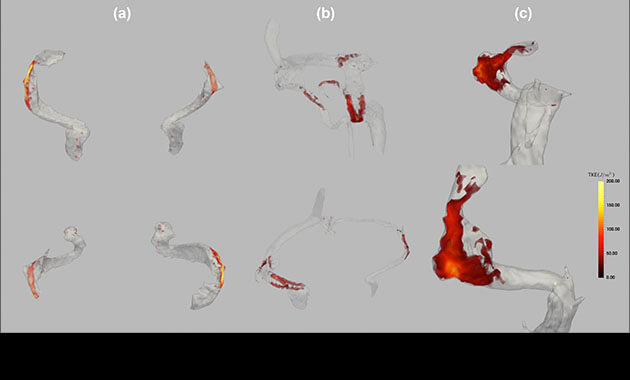
- Brain Aneurysm: A brain aneurysm is a bubble or bubble-like weakening in a blood vessel (artery) of the brain. Aneurysms can cause pulsatile tinnitus because of abnormal blood flow; they also have the potential to leak or rupture, causing bleeding into the brain or its surrounding space (a type of stroke). UCSF offers the full range of treatments for this condition, which includes monitoring with MRI, image-guided interventions, and surgery. UCSF helps more than 300 patients with brain aneurysms each year, and is actively involved in research into the causes, prevention, and treatment of these diseases.
- Venous Sinus Stenosis: Venous sinus stenosis is an abnormal narrowing of a vein in the head carrying blood away from the brain. Sometimes these require treatment by a neurointerventional radiologist to treat the abnormal blood flow.
- Sigmoid Diverticulum: Sigmoid diverticulum is an abnormal outpouching of a vein in the head carrying blood away from the brain. Sometimes these require treatment by a neurointerventional radiologist to treat the abnormal blood flow.
- High Riding Jugular Bulb: High riding jugular bulb refers to a vein that is abnormally close to the hearing organ. Sometimes this can cause pulsatile tinnitus.
Pulsatile Tinnitus FAQs
How serious is pulsatile tinnitus?
Pulsatile tinnitus is a common symptom that impacts between 3-5 million americans. While the potential underlying diseases are many, only some cary significant risks of intracranial hemorrhage, stroke, or blindness. Therefore, evaluation by a specialists with high levels of experience is recommended. In addition, many patients suffer from their pulsatile tinnitus, and in our experience there I usually an underlying structural cause that may be possible to correct and alleviate symptoms.
How does pulsatile tinnitus differs from regular tinnitus?
Pulsatile tinnitus is a rhythmic sound typically in sync with the heartbeat. It is usually described as a whooshing type of noise (fetal heart beat, crescendo-decrescendo quality). Continuous tone tinnitus is quite separate and not usually vascular.
What is the most common cause of pulsatile tinnitus?
Venous sinus stenosis/IIH is the most common cause of pulsatile tinnitus. Dural arteriovenous fistula is the most potentially dangerous cause of pulsatile tinnitus. Our team are experts in the diagnosis and treatments of all causes of pulsatile tinnitus.
Should I see a doctor for pulsatile tinnitus?
Yes. Unfortunately not all physicians are experienced in pulsatile tinnitus, and referral to a high volume institution such as ours may be needed.
When should I worry about Pulsatile Tinnitus?
Pulsatile tinnitus can be a symptom of a dangerous problem with the blood vessels in the head, but not always. Sometimes, pulsatile tinnitus can signal a more serious impending health problem, like a stroke or blindness. Therefore, pulsatile tinnitus should prompt you to see a doctor to further assist you. Pulsatile tinnitus can also significantly impact your mood, and sometimes needs to be treated for this.
Is Pulsatile Tinnitus an emergency?
That depends on what is causing the pulsatile tinnitus. Some causes need to be treated urgently, but most do not. Understanding what is causing the pulsatile tinnitus is key to determining the best course of action.
What happens if Pulsatile Tinnitus Is untreated?
That depends on what is causing the pulsatile tinnitus. If the pulsatile tinnitus is caused by a dangerous problem with the blood vessels in the head or neck, and it is untreated, blindness or stroke (causing problems with walking, talking, or death) can result. A doctor should help you determine whether your pulsatile tinnitus is dangerous or not, and then you can decide whether to leave it untreated or not.
Billing & Insurance
After a procedure is scheduled, UCSF Interventional Neuroradiology will help patients and referring practices with pre-service insurance authorization or pre-service coverage determination when the patient is referred by a UCSF provider.
Multidisciplinary Team
 Matthew Amans, MD
Matthew Amans, MD
Director, Pulsatile Tinnitus Clinic
Associate Professor of Radiology
Neurointerventional Radiology
 Christine Glastonbury, MD
Christine Glastonbury, MD
Professor
Vice Chair, Academic Affairs Radiology
Mentorship Director, ENT Radiology

Wade Smith, MD
Professor
Neurology

Professor
MSBI Program Director
 Charles Limb, MD
Charles Limb, MD
Professor, OHNS
 Kazim Narsinh, MD
Kazim Narsinh, MD
Assistant Professor of Radiology
Neurointerventional Radiology
 Allison Lamboy, NP, MSN
Allison Lamboy, NP, MSN
Nurse Practitioner















 Allison Lamboy, NP, MSN
Allison Lamboy, NP, MSN