Size and Weight Considerations for Imaging and Image-Guided Interventions
Important patient size limitations must be considered when obtaining diagnostic imaging and performing image-guided interventions. These limitations, including patient weight and diameter, vary between imaging modalities (e.g. CT, MRI) and even between equipment within each modality. It is essential to operate imaging equipment within limits not only to ensure high quality imaging, but also to avoid patient harm, staff injury, and equipment malfunction.
This website aims to provide information on the size and weight limitations for UCSF imaging modalities. The limits provided below represent the maximum weight/diameter capacitance of a single piece of equipment with the greatest capacity at each UCSF Health imaging site; these limits are not applicable across modalities (MRI vs. CT) or even within each modality (e.g. different CT scanner models have different specifications). Each imaging modality has additional considerations that may preclude successful imaging, even when patients technically meet the manufacturers’ specified limits. These are described in greater detail in the sections dedicated to each imaging modality. The final evaluation and decision on whether it is safe to proceed with imaging or imaging-guided intervention will be made by the radiology imaging modality managers.
If you are caring for a patient whose size might preclude successful imaging and you would like to discuss this with our UCSF radiology team, please use the contact information provided below.
Imaging Modality Weight and Size Limits
CT Scanners
| Imaging Site | Maximum Weight | Maximum Diameter |
|---|---|---|
| Parnassus Hospital | 450 lbs | 70 cm |
| Parnassus PET/CT | 500 lbs | 78 cm |
| Medical Building 1 400 Parassus (Outpatient) |
450 lbs | 70 cm |
| Mission Bay Hospital | 450 lbs | 80 cm |
| Precistion Cancer Medicine Building (Outpatient) |
675 lbs | 70 cm |
| China Basin (Outpatient) | 450 lbs | 70 cm |
| Mount Zion Hospital | 450 lbs | 70 cm |
| Radiology at 2330 Post Street (Outpatient) |
450 lbs | 70 cm |
| Berkeley Outpatient Center | 500 lbs | 78 cm |
For additional questions about CT scanner diameter and weight limits, please contact:
Jessica Pfannenstiel, CT Manager
Ph: (415) 353-8784
Pager: (415) 443-5411, Voalte
Email: [email protected]
Kimberly Kallianos, MD, CT, Modality Director
Ph: (415) 353-9527 (reading room)
Pager: (415) 443-4737
Email: [email protected]
MRI Scanners
| Imaging Site | Maximum Weight | Maximum Diameter* |
|---|---|---|
| Parnassus Hospital** | 450 lbs*** | 60 cm |
| Medical Building 1 400 Parassus (Outpatient) |
500 lbs | 70 cm |
| Mission Bay Hospital | 550 lbs | 70 cm |
| Precistion Cancer Medicine Building (Outpatient) |
450 lbs | 70 cm |
| China Basin (Outpatient) | 450 lbs | 70 cm |
| Radiology at 2330 Post Street (Outpatient) |
550 lbs | 68 cm |
| Berkeley Outpatient Center | 550 lbs | 70 cm |
*Diameter is often the limiting factor for MRI. Maximum diameter listed does not account for padding and coils necessary for safe and effective imaging. Padding and coils may decrease the maximum patient diameter by up to 5 cm. Please see MRI section for more details.
**There is a protocol for transferring Parnassus inpatients to Mission Bay to obtain imaging when necessary and appropriate. Please see MRI section for more details.
***MRI with 550 lbs weight limit and 70 cm max diameter will be installed at Parnassus campus early 2022. This will obviate the need for transfer of inpatients between Parnassus and Mission Bay.
For additional questions about MRI scanner diameter and weight limits, please contact:
- MRI Operations: (415) 443-5408 (pager)
- Email: [email protected]
Interventional Radiology
| Imaging Site | Maximum Weight |
|---|---|
| Parnassus Hospital | 551 lbs |
| Mission Bay Hospital | 606 lbs |
| Precision Cancer Medicine Building (Outpatient) | 606 lbs |
| Mount Zion Hospital | 444 lbs |
For additional questions about IR table weight limits, please contact:
- Parnassus Hospital: Julio Gonzalez, RT: 415-353-8694
- Mission Bay and Precision Cancer Medicine Building: Vincent Ramirez, RT: 415-476-0266
- Mount Zion Hospital: Joseph Go, RT: 415-502-4562
Neuroendovascular Surgery
| Imaging Site | Maximum Weight |
|---|---|
| Parnassus Hospital | 689 lbs |
| Mission Bay Hospital | 606 lbs |
For additional questions about Neuro IR table weight limits, please contact:
- Parnassus Hospital: Julio Gonzalez, RT: 415-353-8694
- Mission Bay Hospital: Vincent Ramirez, RT: 415-476-0266
Molecular Imaging & Therapeutics
| Imaging Site | Maximum Weight | Maximum Diameter |
|---|---|---|
| Parnassus Hospital | ||
| SPECT/CT* | 500 lbs | 63-65 cm |
| Mission Bay | ||
| SPECT/CT | 450 lbs | 60 cm |
| PET/CT | 385 lbs | 70 cm |
| China Basin | ||
| SPECT/CT | 500 lbs | 63-65 cm |
| PET/CT | 499 lbs | 78 cm |
| PET/MR | 450 lbs | 60 cm |
| Cardiovascular Research Institute | ||
| SPECT/CT | 500 lbs | 63-65 cm |
*Some SPECT machines at the Parnassus site have the capability to perform planar imaging without strict weight limitations. Please see Molecular Imaging section for further details.
For additional questions about SPECT and PET scanner diameter and weight limits, please contact:
Technologist at 415-353-1693 (Parnassus), 415-514-4356 (Mission Bay), or 415-353-3797 (China Basin) or Radiologist in the reading room at 415-353-1692 (Parnassus) or 415-514-4356 (Mission Bay). Alternatively, email [email protected].
Diagnostic X-Ray Radiographs
| Imaging Site | Maximum Weight* |
|---|---|
| Parnassus Hospital Emergency Department |
485 lbs (with table movement) 705 lbs (stationary table) |
| Medical Building 1 400 Parnassus (Outpatient) |
485 lbs (with table movement) 882 lbs (stationary table) |
| Mission Bay Hospital | 486 lbs |
| Precision Cancer Medicine Building (Outpatient) | 485 lbs |
| Mount Zion Hospital | 485 lbs (with table movement) 705 lbs (stationary table) |
*Some diagnostic radiographs can be performed portably. However, this may affect imaging quality and a discussion with an attending radiologist may be necessary. Please see X-ray section for more details.
For additional questions about diagnostic x-ray table weight limits, please contact:
- Parnassus Hospital: Lisa Burke, RT: 415-353-2565
- Mission Bay and Precision Cancer Medicine Building: David Gospe, RT: 415-502-9773
- Mount Zion Hospital: Chester Lim, RT: 415-885-3653
- Orthopedics Institute and Montgomery Street: Jessica Sloss, RT: 415-514-6125
Fluoroscopy Table
| Imaging Site | Maximum Weight |
|---|---|
| Parnassus Hospital | 600 lbs |
| Mission Bay Hospital | 400 lbs |
| Orthopedic Institute | 550 lbs |
| Mount Zion Hospital | 600 lbs |
For additional questions about fluoroscopy table weight limits, please contact:
- Parnassus Hospital: Lisa Burke, RT: 415-353-2565
- Mission Bay Hospital: David Gospe, RT: 415-502-9773
- Mount Zion Hospital: Chester Lim, RT: 415-885-3653
- Orthopedics Institute: Jessica Sloss, RT: 415-514-6125
Breast Imaging (Stereotactic Biopsy Table)
| Imaging Site | Maximum Weight* |
|---|---|
| Precision Cancer Medicine Building (Steriotactic Biopsy Table) |
400 lbs |
*Please see MRI table for size and weight limitations regarding breast MRI imaging and MRI-guided biopsies.
For additional questions about table weight limits in breast imaging, please contact:
Amy Vincent, RT: 415-885-7804
DEXA Scanners
| Imaging Site | Maximum Weight |
|---|---|
| Mount Zion Hospital | 450 lbs |
| Precision Cancer Medicine Building | 450 lbs |
| Orthopedic Institute | 450 lbs |
| UCSF Imaging 1725 Montgomery Street | 450 lbs |
For additional questions about DEXA scanner weight limits, please contact:
- Precision Cancer Medicine Building: David Gospe, RT: 415-502-9773
- Mount Zion Hospital: Chester Lim, RT: 415-885-3653
- Orthopedics Institute and Montgomery Street: Jessica Sloss, RT: 415-514-6125
Ultrasound Imaging
There are no strict weight or size limitations for ultrasound, as patients are imaged in a hospital gurney/bed. However patient size can have important effects on image quality. Please see Ultrasound section below for more details.
Modality Specific Information
Computed Tomography (CT)
Detailed Size & Weight Limitations
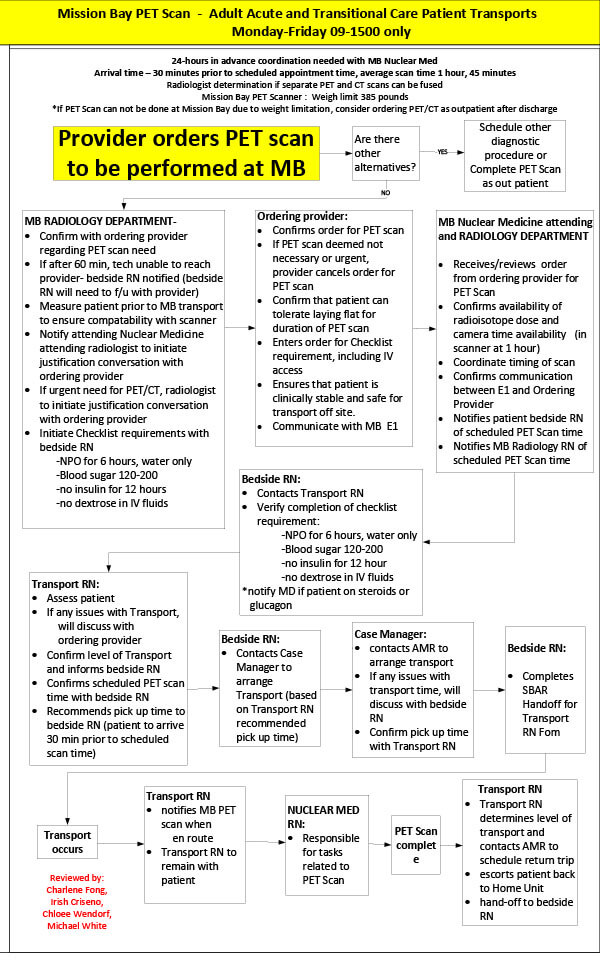
CT scanners have both weight and diameter limits. The patient, or body part of interest, must fit within the CT gantry (doughnut-shaped opening) in both the vertical and horizontal dimensions in order for the scan to occur. It is important to note that the scanner’s vertical diameter is further constrained by the table (as demonstrated by the image below) and must be taken into consideration when determining if a patient will fit into the scanner.
Most CT scans are performed with the patient in a supine position. Patients should be able to lie flat for the duration of the exam. Ideally, CT scans are performed with patients’ arms in an outstretched position over their heads, as this reduces imaging artifacts. This positioning may have variable effects on a patient’s ability to fit into the scanner.
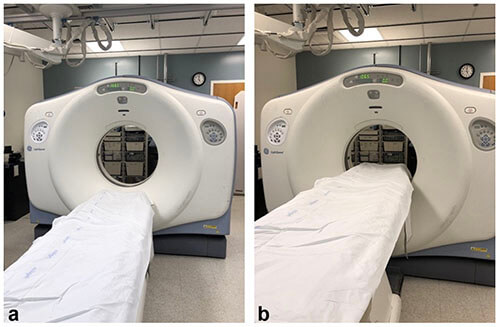
Images demonstrating how the table narrows gantry size, most notably in the vertical dimension.1
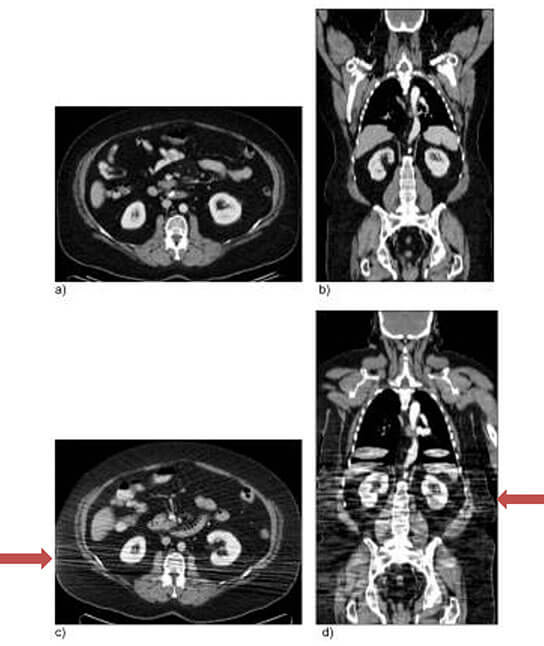
Axial and coronal CT images from a patient scanned positioned with their arms overhead (a,b) versus down by their side (c, d). Beam hardening artifact and decreased image quality result from the improper positioning (c, d).2
Impacts on Image Quality & Radiation Dose
Patient size can impact CT image quality and result in imaging artifacts. Increased tissue thickness results in attenuation of x-rays. Increased attenuation causes images to look “noisy” (i.e., more grainy) in appearance, which may decrease the diagnostic value of the imaging study. Increased thickness also increases the amount of time it takes for the x-ray to penetrate the body. This can result in motion artifact as exposure time increases, also decreasing the diagnostic value of the imaging study. Sometimes imaging parameters can be adjusted to obtain better quality images for large patients, albeit at the cost of increased radiation dose.
If part of a patient’s anatomy extends to the edge of the CT gantry, this can result in beam hardening artifact, which appears as alternating streaks of white and dark lines within adjacent tissues. Beam hardening artifact may obscure findings and limit interpretation of the image.

Axial CT slice showing multiple CT artifacts related to size, including increased noise/quantum mottle throughout the image, beam hardening artifact at the flanks (arrows), and motion artifact, which manifests as indistinct organ margins.1
Magnetic Resonance Imaging (MRI)
Detailed Size & Weight Limitations
While MRI scanners have weight limitations, the bore diameter is most often the limiting factor. The available diameter within the bore is often further reduced by protective padding and imaging coils. Please see “Risks to Patient” section below for further explanation.
For outpatients, radiology schedulers inquire about patients’ weight at the time of scheduling. If the patient’s weight exceeds 260 lbs, the patient is instructed to measure their body diameter to determine whether they will safely fit within the MRI bore. These patients are scheduled at sites with the largest bore diameter. If the patient lives close, or so desires, they may come to the imaging site prior to their appointment for a “fit test.”
For inpatients where MR imaging is urgent, it may be necessary to transfer patients from Parnassus to the Mission Bay Hospital, as the Mission Bay Hospital has a wider bore MRI with a higher weight limit. For details on this transportation protocol, please see Appendix A below. Transferring patients to Mission Bay will no longer be necessary in early 2022, when installation of a wide bore MRI is slated for completion at the Parnassus inpatient hospital.
UCSF does not currently operate any “open MRI” scanners. While “open MRI” scanners exist and can accommodate a larger patient diameter, these scanners are typically of lower magnetic field strength and therefore result in lower image quality when compared to higher field strength MRI scanners with closed bores.
Risks to Patient
Patients should not be “squeezed” into the MRI bore so that their skin is touching the inner lining of the bore, as this can result in serious skin burns. Protective padding or pillows can be placed between the bore and the patient to prevent burns. In addition to protective padding, imaging coils placed on the patient are often necessary to obtain diagnostic quality imaging. These coils further reduce the maximum patient diameter that will fit within the bore. The combination of safety padding and imaging coils may reduce the diameter of the patient that will safely fit within the MRI bore by up to 5 cm (i.e., for a 70 cm bore scanner, 65 cm may be the maximum safe patient diameter). There is also increased potential for claustrophobia as patients’ bodies approach the inner lining of the bore. The decision of whether a patient will safely fit within the scanner is ultimately made by MRI modality managers.
Impacts on Image Quality
Patient size can impact imaging quality and result in artifacts. Increased subcutaneous tissue can result in increased attenuation of radiofrequency waves, ultimately resulting in decreased image quality (lower signal-to-noise). Sometimes this can be mitigated by scanning larger patients at a higher magnetic field strength. Imaging patients with obesity when a body part extends beyond the MRI field of view may result in an artifact that interferes with diagnostic imaging (“wrap-around artifact).”
Interventional Radiology and Image-Guided Interventions
Detailed Size & Weight Limitations
Image-guided interventions are performed using a variety of imaging modalities including fluoroscopy, ultrasound, CT, and MRI. Please refer to each specific modality section for further detail and description regarding size limitations and imaging impact. Decreased image quality can impact the ability to plan and perform image-guided interventions. Difficulties may also arise related to length of the equipment used to perform various interventions. Sometimes this can be mitigated with careful pre-procedure planning.
Risks to Patients
As described in the fluoroscopy section, radiation dose increases with patient size. Complex and long procedures may result in higher patient radiation doses, especially when performed in larger patients under fluoroscopy with angiography. Such patients are at increased risk for skin burns and require close clinical follow-up. UCSF interventional and neurointerventional radiology teams follow a protocol-driven approach for ongoing assessment of these patients when threshold doses are met or exceeded.
Molecular Imaging and Therapeutics
Detailed Size & Weight Limitations
Molecular imaging (formerly nuclear medicine) exams are acquired by single-photon emission computed tomography (SPECT), positron emission tomography (PET), or planar imaging. Because PET and SPECT exams are combined with cross-sectional imaging for improved anatomic localization (CT or MRI), the size and weight limitations of the exam are often determined by the cross-sectional component. Please see the CT and MRI sections for further details.
- Exams acquired with PET include FDG PET, cardiac PET, PSMA PET, and DOTA-TATE PET.
- Exams acquired with SPECT or planar imaging include cardiac perfusion scans, bone scans, V/Q scans, HIDA scans, and others. Please contact the MI&T department if there are further questions about how a specific exam is acquired.
Most molecular imaging scans are performed with the patient supine. Patients should be able to lie flat for the duration of the exam. Most scans are performed with the patients arms in an outstretched position over their head, as this reduces imaging artifacts. This positioning may have effect the patient’s ability to fit into the scanner.
For inpatients at Parnassus where PET/CT imaging is urgent, it may be necessary to transfer patients to the Mission Bay Hospital. For details on this transportation protocol, please see Appendix B below. Transferring patients to Mission Bay will no longer be necessary in 2022, once PET/CT is installed at the Parnassus campus.
Risks to Patients
Patients must completely fit within the SPECT/CT scanner and remain as still as possible during image acquisition. If patients are “squeezed” into the scanner or shift positions during the image acquisition, they may be harmed if the rotating machine contacts them.
Impacts on Image Quality
Certain SPECT cameras can be used to obtain planar imaging while the patient remains in the gurney, therefore avoiding the strict weight limitations of the imaging table. However, this decreases image quality and anatomic localization as cross-sectional imaging cannot be included.
An additional consideration for molecular imaging studies is the dose of radioisotope that can safely be administered. Radioisotope dosing is weight-based and therefore increased doses are required in patients with increased weight to allow for diagnostic imaging. However, there are upper limits to the dose that can be safely administered. A dose reduction required for safety reasons will result in a decreased signal-to-noise ratio and decreased image contrast, ultimately decreasing the imaging quality. In addition, patients with obesity often require longer molecular imaging scan times, which can lead to motion artifact, which may further decrease image quality.

Coronal PET images from three patients of varying diameters and weights (patient weight increases from a to c) demonstrating increased image degradation as patient’s diameter/weight increases.2
Diagnostic X-Ray
Detailed Size & Weight Limitations
Diagnostic x-rays can often be performed portably, with the patient in a bed/gurney, allowing for imaging of patients of almost any size. However, the size of the detector/cassette, may limit the ability to obtain radiographs of larger body areas, such as the chest or abdomen, in a single image.
Weight limits for diagnostic x-ray equipment are variable and depend on whether the table needs to be elevated or if it can be used in a stationary position. The weight limits are reduced by approximately 200 lbs when table movement is required versus stationary table use.
Impacts on Image Quality & Radiation Dose
As with CT, patient size can impact x-ray image quality and result in imaging artifacts. Increased tissue thickness results in attenuation of the x-rays. Increased attenuation causes images to look “noisy” (i.e., more grainy) in appearance, which may decrease the diagnostic value of the imaging study. Increased thickness also increases the amount of time it takes for the x-ray to penetrate the body. This can result in motion artifact as exposure time increases, which may also decrease the diagnostic value of the image. Sometimes imaging parameters can be adjusted to obtain higher quality images, however this often requires increased radiation dose.
Fluoroscopy
Detailed Size & Weight Limitations
Weight limits for fluoroscopy tables differ depending on if the footboard must be used or if the exam requires table movement. Size and weight limitations for fluoroscopy are exam-dependent, because some fluoroscopic exams are performed with the patient standing, while others are performed with the patient lying on the table.
Impacts on Image Quality & Radiation Dose
As with CT and x-ray, patient size can impact x-ray image quality and result in imaging artifacts. Increased tissue thickness results in attenuation of the x-rays. Increased attenuation causes images to look “noisy” (i.e., more grainy) in appearance, which may decrease the diagnostic value of the imaging study. Increased thickness also increases the amount of time it takes for the x-ray to penetrate the body. This can result in motion artifact as exposure time increases, which may decrease the diagnostic value of the imaging study. Sometimes imaging parameters can be adjusted to obtain higher quality images, however this often requires increased radiation dose.
Breast Imaging
Mammography is typically performed with the patient standing or seated and therefore does not have weight limitations. Patients with large breasts may require multiple images to be taken in each projection to adequately include all of the breast tissue.
Breast ultrasound may require modifications in patient positioning and choice of transducer to optimize imaging based on breast size.
Stereotactic core breast biopsies are often performed with the patient lying prone on a specially-made biopsy table. Please see above for stereotactic biopsy table weight limits.
Please see MRI section for detail on size and weight limitations for breast MRI and MRI-guided breast biopsies.
Ultrasound
Impacts on Image Quality
Body habitus impacts ultrasound imaging quality, predominantly as related to the amount and distribution of adipose tissue. Adipose tissue attenuates sound waves, decreasing penetration of the ultrasound beam. Image quality is often worse in patients with a greater amount of subcutaneous, rather than intraperitoneal, adipose tissue. Subcutaneous adipose tissue immediately attenuates the ultrasound beams, hindering their ability to penetrate internal organs. This can have significant clinical impacts. For example, multiple ultrasound exams may be necessary to accurately characterize fetal anatomy in patients with high body mass index
(BMI)3-5.
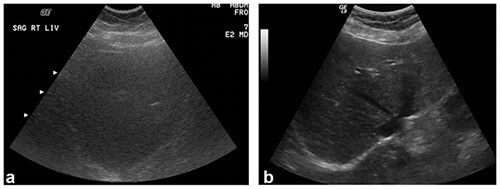
Liver ultrasound images showing increased attenuation of ultrasound beams in a patient weighing 350 lbs (left) compared to a patient weighing 150 lbs (right). Note, the decreased image detail in image (a) as compared to image
(b).1
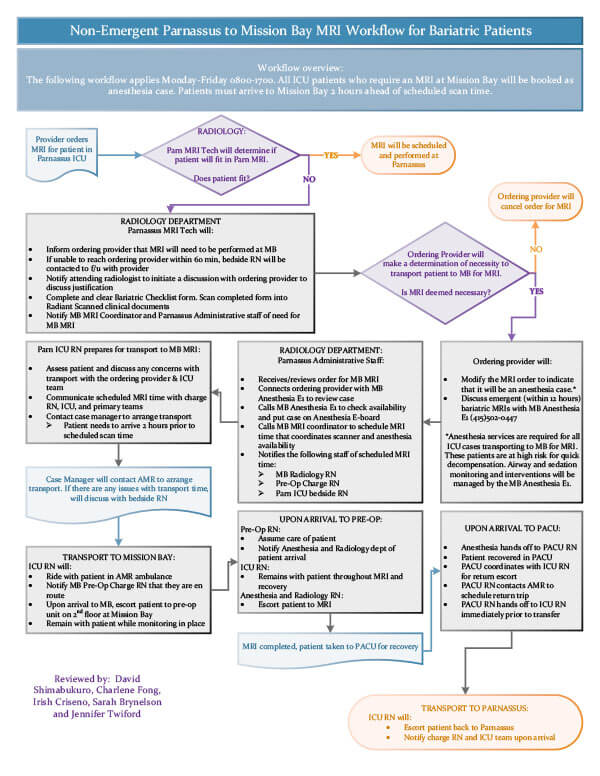
Appendix A: Non-emergent Parnassus to Mission Bay MRI Workflow
As previously mentioned, it may occasionally be necessary to transfer inpatients from the Parnassus Hospital to the Mission Bay Hospital for access to a wider bore MRI with a higher weight limit. Because such transfers are complex processes with multiple stakeholders, this is only done when the medical need for MR imaging prior to discharge from the hospital is clear.
A multidisciplinary UCSF team developed the workflow described below to ensure safe patient transfer and imaging. This workflow temporarily transfers responsibility for the care of transferred patients to the anesthesia service at Mission Bay and is applicable to both ICU and non-ICU patients. The workflow also clarifies responsibilities of the ordering and radiology teams regarding confirming anesthesia and MRI scanner availability and facilitating transfer. Such cases are only scheduled Monday through Friday from 8 am to 5 pm, based on radiology and anesthesia availability.
This workflow will no longer be necessary in early 2022, when installation of a wide bore MRI is slated for completion at the Parnassus inpatient hospital.
Appendix A: Non-emergent Parnassus to Mission Bay MRI Workflow (pdf)
Appendix B: Non-emergent Parnassus to Mission Bay PET/CT Workflow
As previously mentioned, it may occasionally be necessary to transfer inpatients from the Parnassus Hospital to the Mission Bay Hospital for access to PET/CT. Because such transfers are complex processes with multiple stakeholders, this is only done when the medical need for PET/CT imaging prior to discharge from the hospital is clear.
A multidisciplinary UCSF team developed the workflows described below to ensure safe patient transfer and imaging. For ICU patients, this workflow temporarily transfers responsibility for the care of transferred patients to the anesthesia service at Mission Bay. This workflow also clarifies responsibilities of the ordering and radiology teams regarding scanner and radioisotope availability, patient preparation, facility transfer and anesthesia availability for ICU patients. Please note that cases, for both ICU and non-ICU level patients, are only scheduled Monday through Friday from 9 am to 3 pm.
This workflow will no longer be necessary in early 2022, when installation of a PET/CT scanner is slated for completion at the Parnassus inpatient hospital.
References
- Uppot RN. Technical challenges of imaging & image-guided interventions in obese patients. Br J Radiol. 2018;91(1089):20170931.
- Blodgett TM, Mehta AS, Mehta AS, Laymon CM, Carney J, Townsend DW. PET/CT artifacts. Clin Imaging. 2011;35(1):49-63.
- Simmons PM, Wendel MP, Whittington JR, San Miguel K, Ounpraseuth ST, Magann EF. Accuracy and completion rate of the fetal anatomic survey in the super obese parturient. J Ultrasound Med. Published online December 5, 2020.
- Hendler I, Blackwell SC, Bujold E, et al. Suboptimal second-trimester ultrasonographic visualization of the fetal heart in obese women: should we repeat the examination? J Ultrasound Med. 2005;24(9):1205-1209; quiz 1210-1211.
- Pasko DN, Wood SL, Jenkins SM, Owen J, Harper LM. Completion and sensitivity of the second-trimester fetal anatomic survey in obese gravidas. J Ultrasound Med. 2016;35(11):2449-2457.