Biomechanics and Musculoskeletal Imaging Lab (Souza Lab)

The Biomechanics and Musculoskeletal Imaging Lab (BMIL) is dedicated to the investigation of biomechanics associated with lower extremity orthopedic pathology. We use 3D motion analysis, quantitative MRI, multi modal dynamometry and EMG to understand predictors of disease progression. The Director, Dr. Richard Souza, PT, PhD, is the Vice Chair for Research and Professor in the Department of Physical Therapy and Rehabilitation Science. The team consists of clinicians (including physical therapists, sports medicine physicians, and radiologists), engineers, exercise physiologists, and computer scientists. The goal of this lab is to identify and evaluate potential prevention and rehabilitation tools for the treatment of patients with lower extremity orthopedic pathology. We are funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases, the Orthopaedic Research Education Foundation, and the California Physical Therapy Association PT Fund.
Research Projects
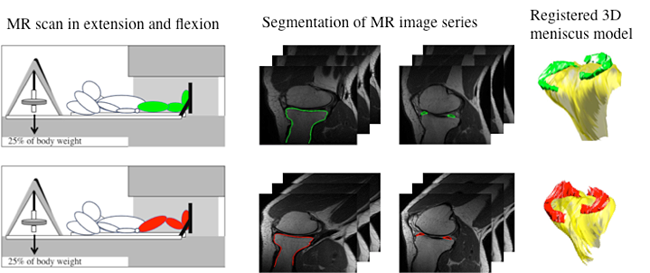
Knee Osteoarthritis: Meniscus Kinematics and Articular Cartilage Degeneration
Osteoarthritis (OA) onset and progression is thought to be related to altered mechanical loading during daily activities. A fibrocartilagenous structure within the knee called the meniscus serves to distribute load across the joint to protect the underlying articular cartilage and bone. The meniscus is known to move as the knee flexes and extends, however abnormal meniscal movement during tasks such as walking and other activities of daily living may play an important role in the onset and progression of knee OA. Advanced quantitative magnetic resonance imaging (MRI) techniques may be used to evaluate meniscal motion, cartilage compositional changes, joint contact mechanics, and radiological grading of disease severity.
Therefore, the purpose of this project is to perform both cross-sectional (OA vs. controls) and longitudinal (3 times over two years) studies of meniscal motion in relationship to cartilage biochemistry. One hundred subjects with and without knee OA have been enrolled to complete kinematic-MRI and relaxation time mapping for cartilage and meniscus composition. Characterizing meniscal kinematics in participants with knee OA will improve out understanding of the mechanisms behind the incidence and progression of knee OA. This knowledge may be directly translated to the clinical setting since altered meniscal movement and morphology may be treated through surgical intervention, and targeting treatment specifically to those individuals that have the greatest risk for cartilage degeneration.
This research is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 1R01AR062370 (PI: Souza) and 1F32AR064129 (PI: MacLeod). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Muscle Adiposity, Function, and Performance in Knee Osteoarthritis
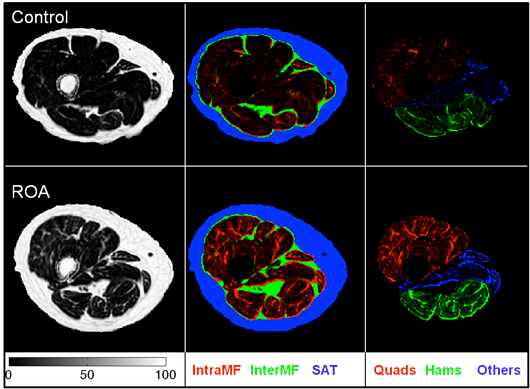
Fat Fractions for control subjects (Black) and OA (Grey) with 95% CI for quadriceps muscle, hamstrings muscle, all remaining muscles and global compartments. (b) Lean Anatomical Cross-sectional area control subjects (Black) and OA (Grey) with 95% CI for quadriceps muscle, hamstrings muscle, all remaining muscles and global compartments. Brackets indicate significant differences at P < 0.05.
It is well known that obesity has a strong association with the risk of development and worsening of knee osteoarthritis. Weakness of the thigh muscles, especially the Quadriceps is a ubiquitous finding in people with knee OA. Loss of muscle tissue only partly explains the loss of strength in people with OA and fatty infiltration of thigh skeletal muscle is known to affect muscle strength and mobility in the elderly. However, little attention has been paid to the changes in fatty- infiltration of the thigh muscles in people with knee osteoarthritis. Using cutting-edge chemical shift-based water/fat separation MRI methods, including Dixon techniques and the iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL), we are investigating the changes in thigh muscle size and adiposity in people with knee osteoarthritis. Furthermore, we are also investigating the association of thigh muscle size and adiposity with cartilage degeneration, muscle performance, and patient symptoms, function, and biomechanics. The project is currently funded by two grants from NIH-NIAMS (PI: Dr. Richard Souza, PI: Dr. Sharmila Majumdar).
Changes in Tibiofemoral Kinematics and Articular Cartilage Before and After Meniscectomy
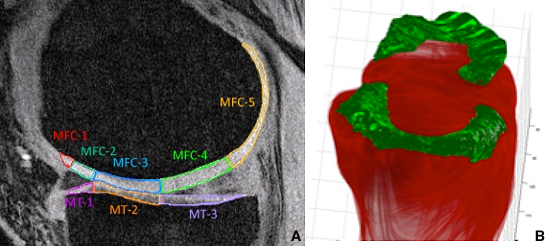
A) Subcompartmental analysis of the medial femoral condyle and tibia. B) 3D rendering of meniscus.
The medial and lateral meniscus are crescent-shaped fibrous pads of the knee joint that provide shock absorption, pressure redistribution, and joint stability contributing to the smooth motion of the knee. However, meniscus tears are among the most common injuries seen by orthopaedic surgeons, and meniscectomy is the most common orthopaedic procedure performed in the United States.
While studies have shown that meniscus tears and partial meniscectomy result in histological changes in articular cartilage and altered tibiofemoral kinematics, it is still unclear if the cartilage changes seen following surgery are a result of the original meniscus tear itself, the partial meniscectomy, or other factors.
This study utilizes state-of-the-art MR techniques to monitor knee cartilage composition with changes in load across the knee joint. Patients who electively undergo meniscectomy will be evaluated before the meniscus surgery and after the surgery to see the effects on the load of the knee.
The results of this study are necessary to determine how changes in mechanical load across the knee results in biochemical changes in the cartilage. Outcomes from our study could potentially allow clinicians to see sub-clinical early osteoarthritis following meniscus injury and provide a way to measure therapeutic interventions before it is irreversible
Gait Retraining to Reduce Knee Pain and Improve Function in Osteoarthritic Patient
The angle of an individual’s feet while walking may place exaggerated stress on certain portions of the knee joint, particularly the medial compartment. This exaggerated load leads to altered movement and cartilage degeneration of the knee which may eventually lead to osteoarthritis. The Gait Retraining Pilot is an interventional study that aims to change the way participants walk in order to reduce loading on the medial compartment of the knee joint. The knee adduction moment (KAM) is a biomechanical variable used to measure this amount of loading on the joint, and is linked to the severity of knee pain in people with Osteoarthritis. The cartilage degeneration resulting from high KAM’s can be visualized using T1ρ and T2 relaxation times from MRI.
In a recent study, it was found that a subtle 7 degree change in the foot progression angle (amount of toe-in) can reduce the KAM during walking by 20%, and show a dramatic improvement in both pain and function in persons with moderate knee OA. However, it remains unknown if this intervention may result in improvements (or less decline) in cartilage composition, as quantified by T1ρ and T2 relaxation times. In addition, the effects of gait retraining on the kinematics and kinetics during similar, but different tasks (such as stair climbing), has not been explored.
Therefore, the objective of this study is to determine the effects of 2, six week long, gait retraining interventions (a moderate 7 degree toe-in modification, and a mild 2 degree toe-in modification) on cartilage composition, muscle and joint morphology, pain, function, and kinematics and kinetics during functional tasks in persons with symptomatic and radiographic knee OA.
2-D Running Analysis Write-up
When measured from multiple angles, 2-dimesional video can give great insight into running mechanics, allowing for a frame-by-frame biomechanical analysis. Variables which dictate running patterns (such as overstride, thigh extension, footstrike, and heel whip) can be reliably measured and quantified. Once gathered, the correlation between these components can be calculated and used to make predictions about the effect of each.
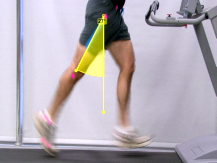
Peak Thigh Extension
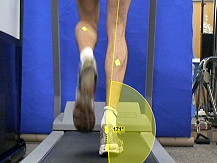
Peak Ankle Eversion

Overstride Angle
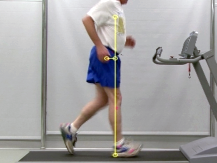
Overstride Distance (Normal)

Overstride Distance (Excessive)
Publications
A complete list of Souza publications can be found at the bottom of Richard Souza's profiles page.
People

Richard B. Souza, PT, PhD, ATC, CSCS
Director
[email protected]
Dr. Souza is a physical therapist and research scientist with expertise in the biomechanical analysis of lower extremity orthopaedic pathology. He obtained his B.S. in exercise science from the University of California, Davis in 1998, and his Master’s degree in physical therapy from Samuel Merritt College in 2002. In 2008, he received his Ph.D. in biokinesiology (major field: biomechanics) from the University of Southern California. His doctoral dissertation was titled “The Influence of Abnormal Hip Kinematics on Patellofemoral Joint Dysfunction.” He joined UCSF Department of Radiology and Biomedical Imaging in May 2008 as a postdoctoral scholar, funded by the National Space and Biomedical Research Institute to investigate the influence of non-weight-bearing on articular cartilage biochemistry. He is currently the Vice Chair for Research and a Full Professor with joint appointments in Physical Therapy and Rehabilitation Science, Radiology and Biomedical Imaging, and Orthopaedic Surgery. His research interests are focused on advanced quantitative magnetic resonance imaging of the lower extremity and biomechanics of human movement. He is involved in projects that evaluate the influence of loading behavior on cartilage health and to determine effectiveness of prevention and rehabilitation strategies on tissue biochemistry.
 Alyssa Bird
Alyssa Bird
PhD Student
[email protected]
Alyssa obtained her B.S. in Kinesiology with a concentration in Exercise Science from California Polytechnic State University, San Luis Obispo in 2017. Later that year, she joined the Department of Physical Therapy and Rehabilitation Science as part of the first Ph.D. in Rehabilitation Science cohort. Alyssa is currently specializing in musculoskeletal biomechanics, focusing her research interests on the relationship between lower extremity pathologies such as hip osteoarthritis and joint health. Her current research utilizes motion analysis and quantitative magnetic resonance imaging to investigate the role of joint loading and tissue health in the development and progression of hip osteoarthritis.
 Tzu-Chieh (Jennifer) Liao, PT, PhD
Tzu-Chieh (Jennifer) Liao, PT, PhD
Postdoctoral Fellow
[email protected]
Dr. Liao is a biomechanist and physical therapist with expertise in lower extremity biomechanics. She received her Ph.D. in Biokinesiology from University of Southern California in 2017. Her doctoral dissertation was titled “The influence of tibiofemoral kinematics and kinetics on patella cartilage stress: a comparison of recreational runners with and without patellofemoral pain.” She is currently a Postdoctoral Scholar in the Musculoskeletal Quantitative Imaging Research Group in the UCSF Department of Radiology. Her research interest lies in identifying the biomechanical factors contributing to musculoskeletal pathology, quantifying disease development and progression through advanced imaging, and with an exploration of the efficacy of the treatment. She is currently involved in projects that evaluate the natural etiology of hip osteoarthritis and the development of knee osteoarthritis following anterior cruciate ligament surgery.
 Carla Kinnunen
Carla Kinnunen
Clinical Research Coordinator
[email protected]
Carla Kinnunen obtained her B.S. in Behavioral Neuroscience from University of San Diego in 2017. In July 2017, she joined the Musculoskeletal Quantitative Imaging Research Group in the UCSF Department of Radiology and Biomedical Imaging as a summer research student. Her work focused on understanding the correlation between intramuscular fat in gluteus muscles and hip pathologies like femoroacetabular impingement through use of quantitative magnetic resonance imaging. She was later hired on as a Staff Research Associate to continue her student work. In September 2018 she transitioned to Clinical Research Coordinator and coordinates various studies focusing on osteoarthritis.
 Tijana Popovic, MS
Tijana Popovic, MS
Staff Research Associate
[email protected]
Tijana received her Master’s degree in Exercise, Fitness, and Health Promotion (major field: biomechanics) from the George Mason University, Virginia in 2016. She served as a graduate research and undergraduate teaching assistant at GMU for two years and has been involved with several studies in Sport Medicine Assessment Research & Testing (S.M.A.R.T.) Laboratory. She completed her Master’s thesis titled “The effect of reduced relative implicit and explicit feedback on lower extremity jump-landing mechanics.” Tijana joined the Musculoskeletal Quantitative Imaging Research Group at the UCSF Department of Radiology and Biomedical Imaging in October 2016 as a Staff Research Associate II. Her research interests focus on development and progression of hip osteoarthritis with the aid of advanced quantitative MRI and motion analysis.
 Koren Roach, PhD
Koren Roach, PhD
Postdoctoral Fellow
[email protected]
Dr. Roach is a biomedical engineer with expertise in lower-limb biomechanical analyses. Dr. Roach earned a B.S. in biomedical engineering at Worcester Polytechnic Institute in 2004. Following graduation, she worked in industry for several years designing medical devices that ranged from advanced energy laproscopic devices and cardiac ablation catheters to orthopaedic instruments for total joint replacement surgery. In 2018, Dr. Roach earned a Ph.D. in biomedical engineering at the University of Utah. Her graduate research focused on the implementing a dual fluoroscopy system to determine three-dimensional motion of bones in the foot and ankle. Foot and ankle biomechanics have been an under-investigated line of research due to the anatomical complexity of the foot and ankle and the advanced imaging techniques required to accurately measure bone motion in this region. Dr. Roach joined the UCSF Department of Radiology and Biomedical Imaging in 2018 as a Postdoctoral Scholar. Her current research is focused on applying innovative time-series analysis techniques to gait biomechanics to develop machine learning models that can accurately predict early-stage hip OA.
Director of BMIL
- Research Directory
- Abdominal Imaging Research
- Abdominal and Pelvic MRI
- Arthritis Imaging Lab (Li Lab)
- Baby Brain Research Group
- Biomagnetic Imaging Laboratory
- Biomechanics & Musculoskeletal Imaging Lab
- Bone Quality Research Lab
- Brain Arteriovenous Malformations
- BrainChange Study
- Breast Imaging Research Group
- Breast and Bone Density Group
- Cardiothoracic Imaging Imaging Research
- Center for Molecular and Functional Imaging (CMFI)
- Contrast Material and CT Translational Research Lab
- Daniel B. Vigneron Lab
- Evans Lab
- Focused Ultrasound Lab
- High Field MRI Center
- Imaging Research for Neurodevelopment
- Interventional Radiology Research Lab
- Larson Group
- Lupo Lab
- Majumdar Lab
- Molecular Imaging Lab (Flavell Lab)
- Multimodal Metabolic Brain Imaging
- Musculoskeletal Magnetic Resonance Imaging Lab (Krug Lab)
- Musculoskeletal Quantitative Imaging Research
- Neural Connectivity Lab
- Neuroradiology Research
- Osteoid Osteomas HIFU Clinical Trial
- PET/SPECT Radiochemistry
- PSMA PET Scan
- Pediatric Research
- Physics Research Laboratory
- Program for Molecular Imaging and Targeted Therapy
- Prostate Cancer Imaging Lab (Kurhanewicz)
- Research
- Sarah J. Nelson Lab
- Surbeck Laboratory
- Translational Metabolic Imaging Lab
- UCSF Nuclear and Clinical Molecular Imaging Research
- Vascular Imaging Research Center
- Viswanath Ronen Lab
- Wilson Lab
- Imaging Research Symposium
- Research Conference
- UCSF Radiology at RSNA
- Core Services
BMIL Contact
185 Berry Street, Suite 350
San Francisco, CA 94107
Phone: (415) 514-8930
Fax: (415) 353-3438
Email: [email protected]